What is Alcoholic Cirrhosis?
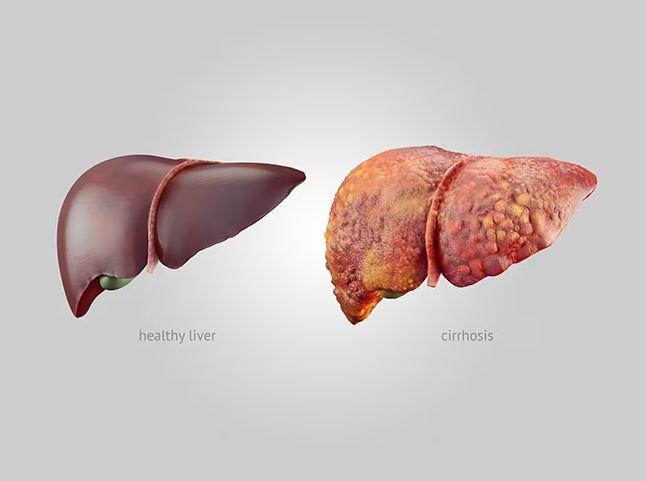
Alcoholic cirrhosis is a progressive liver disease that occurs as a result of long-term and excessive alcohol consumption. It is the most common type of cirrhosis in many countries where alcohol abuse is prevalent. Cirrhosis refers to the scarring and damage of the liver tissue, which leads to the loss of its typical structure and function.
In alcoholic cirrhosis, it accumulates scar tissue, gradually replacing healthy liver tissue and impairing the liver’s ability to carry out its crucial tasks. As cirrhosis progresses, liver function declines, and complications can arise.
Alcoholic Liver Cirrhosis Symptoms
Alcoholic liver cirrhosis is a late-stage liver disease caused by long-term and excessive alcohol consumption. The symptoms of alcoholic liver cirrhosis can differ from patient to patient, but here are a few common symptoms associated with this condition:
- Fatigue and weakness: Feeling tired and lacking energy is a common symptom of liver disease, including alcoholic cirrhosis.
- Jaundice: This is characterized by a yellowing of the eyes and skin due to the accumulation of bilirubin, a pigment made by the liver. Jaundice may occur in individuals with cirrhosis, indicating liver dysfunction.
- Loss of appetite and weight loss: Cirrhosis can reduce appetite, resulting in unintended weight loss.
- Nausea and vomiting: Liver dysfunction can cause digestive issues such as nausea and vomiting.
- Abdominal pain and tenderness: Some individuals with alcoholic cirrhosis may experience pain or discomfort in the upper right area of the abdomen.
- Swelling in the legs: Cirrhosis can lead to fluid retention, resulting in swelling in the ankles and legs, known as peripheral edema.
- Mental confusion and changes in behavior: Advanced liver disease can affect brain function, leading to confusion, difficulty concentrating, memory problems, and changes in behavior or mood. This condition is known as hepatic encephalopathy.
- Spider-like blood vessels (spider angiomas): These are small, dilated blood vessels that may appear on the skin, especially on the upper body, chest, and face.
- Easy bruising and bleeding: Cirrhosis can affect the production of blood clotting factors, leading to easy bruising and prolonged bleeding.
- Palmar erythema: The palms of the hands may appear reddened or flushed.
These alcoholic cirrhosis symptoms can vary in severity and may be influenced by individual factors such as the extent of liver damage and overall health. If you or someone you’re concerned with is experiencing symptoms related to liver disease, it is crucial to seek medical attention for a proper diagnosis and appropriate management.
Causes of Alcohol Cirrhosis of the Liver
Alcohol cirrhosis, also known as alcoholic liver cirrhosis, is a condition characterized by severe scarring and damage to the liver due to long-term alcohol abuse. The primary cause of alcoholic cirrhosis is the excessive and prolonged consumption of alcohol.
Here are a few critical aspects that contribute to the development of alcohol cirrhosis:
- Quantity and duration of alcohol consumption: Alcohol cirrhosis typically occurs in individuals who have been heavy drinkers for many years. Prolonged and excessive alcohol consumption is a significant risk factor for developing liver cirrhosis.
- Metabolism of alcohol: When alcohol is consumed, it is primarily metabolized in the liver. The liver breaks down alcohol into various byproducts, including toxic substances that can damage liver cells. Chronic and excessive alcohol consumption overwhelms the liver’s ability to metabolize alcohol, leading to liver damage over time.
- Genetic factors: Some individuals may be more susceptible to alcohol-related liver damage due to genetic factors. Certain genetic variations affect how alcohol is metabolized, making some people more vulnerable to the toxic effects of alcohol on the liver.
- Gender: Women generally have a higher risk of developing alcoholic cirrhosis compared to men. This is partly because women tend to have lower levels of certain enzymes involved in alcohol metabolism, leading to higher alcohol concentrations and increased liver damage.
- Nutrition: Poor nutrition, particularly a deficiency in essential vitamins and minerals, can contribute to developing and progressing alcoholic cirrhosis. Alcohol abuse often leads to malnutrition as alcohol interferes with the absorption and utilization of essential nutrients.
- Other liver diseases: Alcohol consumption can exacerbate the effects of other liver diseases, such as viral hepatitis (hepatitis B or C), leading to a higher risk of developing cirrhosis.
All heavy drinkers will develop alcohol cirrhosis, as individual susceptibility can vary. However, the above list of risk factors significantly increases the risk of developing this condition.
Alcohol and Cirrhosis Complications
Alcohol abuse and cirrhosis can lead to severe complications that significantly impact a person’s health. Chronic alcohol consumption can cause liver cirrhosis, a condition characterized by extensive scarring and damage to the liver tissue.
Cirrhosis can also lead to fluid accumulation in the abdominal cavity (ascites), impair brain function (hepatic encephalopathy), and disrupt the liver’s ability to produce clotting factors, leading to coagulation disorders. These complications can profoundly impact the overall well-being and prognosis of individuals with alcohol-related cirrhosis, underscoring the significance of seeking medical help and support for alcohol abuse.
Skip To:
Learn More:
- Risks Of Alcoholic Hepatitis vs Cirrhosis
- Alcoholic Hepatitis Symptoms, Signs, & Causes
- Alcoholic Wet Brain Symptoms, Wernicke-Korsakoff Syndrome/Wet Brain Syndrome Meaning, Stages, Effects & Treatment.
- Alcoholic Organic Brain Syndrome Symptoms & Treatment
- Symptoms & Signs Of A High Functioning Alcoholic
- How to Help a High Functioning Alcoholic?
- How to Help an Alcoholic? Alcoholic Recovery Tips & Support
- Alcohol Induced Dementia Symptoms & Treatment
- Alcohol Detox Timeline & How To Safely Manage Alcohol Withdrawal Symptoms Treatment
- What is Alcohol Induced Psychosis? Symptoms & Treatment
Get Help. Get Better. Get Your Life Back.
Searching for Accredited Drug and Alcohol Rehab Centers Near You?
Even if you have failed previously and relapsed, or are in the middle of a difficult crisis, we stand ready to support you. Our trusted behavioral health specialists will not give up on you. When you feel ready or just want someone to speak to about therapy alternatives to change your life call us. Even if we cannot assist you, we will lead you to wherever you can get support. There is no obligation. Call our hotline today.
(844) 597-1011Alcohol Liver Cirrhosis Stages
Alcoholic liver cirrhosis can be categorized into several stages based on the extent of liver damage and disease progression. The stages are as follows:
- In this stage, the liver still retains some functioning despite cirrhosis.
- The symptoms of cirrhosis from alcohol may be mild or absent, and liver function tests may show only slight abnormalities.
- The liver can still perform its essential functions, although some damage and scarring are present.
- The liver function has significantly deteriorated in this stage, and complications arise.
- Symptoms, including fatigue, jaundice, abdominal pain, and swelling, become more noticeable.
- Liver function tests show further abnormalities, and the liver’s ability to perform its functions is significantly impaired.
- The development of complications such as ascites (fluid accumulation in the abdomen) and hepatic encephalopathy (brain dysfunction) is more likely.
- This is the most severe stage of alcoholic liver cirrhosis, indicating significant liver dysfunction and decompensation.
- Liver function is severely compromised, and symptoms are pronounced and debilitating.
- Individuals in this stage may experience severe fatigue, jaundice, abdominal pain, significant fluid retention (ascites), hepatic encephalopathy, and increased susceptibility to infections.
- Liver function tests show marked abnormalities, and the liver’s ability to perform its essential functions is severely impaired.
Seeking medical attention, abstaining from alcohol, and receiving appropriate treatment and support are crucial to managing the liver cirrhosis alcohol disease stages and potentially improving outcomes.

Death End Stage Alcoholic Cirrhosis
The death stage of alcoholic cirrhosis is an advanced and end-stage disease with severe and life-threatening liver damage. During this cirrhosis of the liver alcoholic stage, the liver has sustained significant scarring (fibrosis) due to long-term alcohol abuse, leading to impaired liver function and complications that can be fatal. Common complications that contribute to the death stage of alcoholic cirrhosis include the following:
- Liver failure.
- Portal hypertension and variceal bleeding.
- Hepatic encephalopathy.
- Ascites and infections.
- Renal failure.
The death stage of alcoholic cirrhosis is a critical and life-threatening condition. Seeking immediate medical assistance is vital.
Alcoholic cirrhosis, compared to the risk factors for non alcoholic cirrhosis of liver, includes obesity, type 2 diabetes, metabolic syndrome, high blood pressure, high cholesterol, viral hepatitis, autoimmune diseases, and certain medications.
Both forms of cirrhosis can lead to severe health complications, such as liver failure, portal hypertension, and an increased risk of liver cancer. Prompt diagnosis, appropriate management, and lifestyle changes are essential in managing alcoholic and liver cirrhosis non alcoholic conditions.
Alcohol Cirrhosis of Liver Fact Sheet
Alcoholic Hepatitis vs Cirrhosis
Alcoholic hepatitis and cirrhosis are two distinct but closely related conditions that can occur due to excessive alcohol consumption. Here are the critical differences between alcoholic hepatitis and cirrhosis:
Alcoholic Hepatitis:
- Inflammation: Alcoholic hepatitis is characterized by inflammation in the liver caused by alcohol abuse. It is often a reversible condition if alcohol consumption is stopped promptly.
- Shorter-term damage: Alcoholic hepatitis typically develops over a shorter period, ranging from weeks to years of heavy drinking.
- Symptoms: Common symptoms include jaundice (yellowing of the skin and eyes), abdominal pain, enlarged liver, loss of appetite, and sometimes fever.
- Reversible potential: With complete abstinence from alcohol and appropriate medical management, alcoholic hepatitis can improve, and liver function can recover in some cases.
- Progression to cirrhosis: Alcoholic hepatitis can progress to cirrhosis if alcohol consumption continues. Not everyone with alcoholic hepatitis will develop cirrhosis, but it is a possibility if alcohol abuse persists.
Cirrhosis vs Alcoholic Hepatitis:
- Scarring and irreversible damage: Cirrhosis is a chronic condition characterized by extensive liver scarring (fibrosis). The scar tissue replaces healthy liver cells, impairing liver function irreversibly.
- Long-term damage: Cirrhosis typically develops over a more extended period, often after many years of heavy and prolonged alcohol abuse.
- Symptoms: Liver cirrhosis symptoms alcohol causes can include those of alcoholic hepatitis, but additional complications such as ascites (abdominal fluid accumulation), portal hypertension, hepatic encephalopathy, and coagulation disorders may also be present.
- Irreversible: Unlike alcoholic hepatitis, cirrhosis is generally considered irreversible. However, further damage can be prevented and managed by abstaining from alcohol and receiving appropriate medical care.
- Increased risk of liver failure: Cirrhosis increases the risk of liver failure and complications like hepatocellular carcinoma (liver cancer).
- Transplant consideration: In severe cases of cirrhosis with liver failure, transplantation may be the only liver treatment option.
Alcoholic Cirrhosis of Liver with Ascites
In alcoholic cirrhosis, the liver undergoes extensive scarring and loses its ability to function correctly. As a result, blood flow through the liver becomes obstructed, leading to increased pressure in the portal vein. Portal hypertension, in turn, causes fluid to accumulate in the abdominal cavity, resulting in ascites.
Ascites in alcoholic cirrhosis can cause abdominal swelling and discomfort. As the fluid volume increases, it can lead to increased abdominal pressure, reduced lung expansion, and difficulty breathing. Furthermore, ascites increase the risk of bacterial peritonitis, a severe infection of the peritoneal cavity that requires immediate medical attention.
Alcoholic Cirrhosis Bruising Pictures
Alcoholic cirrhosis of the liver is characterized by extensive scarring (fibrosis) and damage to the liver tissue due to chronic and excessive alcohol consumption. Visually, alcoholic cirrhosis may present with several noticeable signs and symptoms.
Early Signs of Cirrhosis of the Liver from Alcohol
In the early stages of liver cirrhosis caused by alcohol abuse, there may not be noticeable symptoms or signs. However, some early signs of alcohol cirrhosis may be present, including the following:
- Fatigue.
- Loss of appetite.
- Nausea and digestive issues.
- Abdominal discomfort.
- Jaundice.
The early symptoms of liver cirrhosis from alcohol can be subtle, easily overlooked, and may not be specific to cirrhosis. If you have an alcohol use disorder history and are experiencing any of these symptoms, seeking medical attention for a proper evaluation and diagnosis is crucial. Early detection and intervention are vital in managing cirrhosis and preventing further liver damage.

Get Your Life Back
Find Hope & Recovery. Get Safe Comfortable Detox, Addiction Rehab & Dual Diagnosis High-Quality Care.
Hotline(844) 597-1011Alcoholic Cirrhosis Disability & Statistics
Living with a chronic and potentially life-threatening condition like alcoholic cirrhosis can cause emotional distress, anxiety, depression, and decreased overall well-being. These emotional and psychological challenges can further contribute to disability and impaired functioning.
Alcoholic cirrhosis can have substantial social and economic consequences. It can lead to reduced productivity, increased healthcare costs, and the need for disability benefits or assistance programs. Early detection, intervention, and adherence to medical management, including abstinence from alcohol, can significantly help prevent further severe complications from alcohol cirrhosis symptoms.
20%
Between 10 and 20 percent of heavy alcohol drinkers will develop cirrhosis condition. Alcoholic liver cirrhosis is the most advanced type of liver disease related to drinking alcohol.
Source: NCBI
1.3%
In 2016. alcohol-related liver cirrhosis accounted for approximately 1.3 percent of all deaths globally.
Source: WHO
47,000
In 2019, chronic liver disease and cirrhosis, including alcoholic cirrhosis, accounted for over 47,000 deaths in the United States.
Source: CDC
Alcoholic Cirrhosis Prevention
Prevention is significant in lowering the risk of developing alcoholic cirrhosis. Here are some critical steps to prevent alcoholic cirrhosis:
- Limit alcohol consumption.
- The most effective way to prevent alcoholic cirrhosis is to avoid excessive and prolonged alcohol consumption. The CDC recommends that individuals should limit their alcohol intake to moderate levels, which means up to 1 glass of drink per day for females and up to 2 glasses per day for males.
- Seek help for alcohol abuse.
- If you have an alcohol use disorder, seeking help from healthcare professionals, support groups, or addiction treatment programs is necessary. They can provide guidance, counseling, and support to help you overcome alcohol dependency and prevent further liver damage.
- Build a support network.
- Surround yourself with a supportive family, friends, or support groups who can assist you in maintaining sobriety and making healthier lifestyle choices.
- Improve overall health.
- Enhancing or improving your overall health can help reduce the risk of alcoholic cirrhosis. This involves eating a well-balanced diet, exercising regularly, maintaining a healthy weight, and managing other medical conditions like high blood pressure and diabetes.
- Regular health check-ups.
- It is significant to have regular medical check-ups with your healthcare provider. They can assess your liver function, monitor for any signs of liver damage, and provide appropriate guidance and interventions. While alcoholic cirrhosis is directly linked to alcohol abuse, non alcoholic liver cirrhosis can develop in individuals without a history of alcohol consumption but with underlying conditions or risk factors.
- Vaccinations.
- Hepatitis A and B vaccines are obtainable and highly recommended for individuals at risk of alcoholic cirrhosis. These vaccines can prevent viral hepatitis, worsening liver damage in individuals with alcoholic cirrhosis.
Remember that prevention is always better than treatment, and making healthy lifestyle choices and seeking help for alcohol abuse is vital to preventing alcoholic cirrhosis. If you or someone you’re concerned with is struggling with alcohol addiction, seeking professional service and support is crucial for a healthier future.
First-class Facilities & Amenities
World-class High-Quality Addiction & Mental Health Rehabilitation Treatment
Rehab Centers TourRenowned Addiction Centers. Serene Private Facilities. Inpatient rehab programs vary.
Addiction Helpline(844) 597-1011Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Success Stories Across Our Network
- Low Patient to Therapist Ratio
- Onsite Medical Detox Center
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Personal Development Events
Alcoholic Cirrhosis Treatment
Individuals with alcoholic cirrhosis must receive regular medical monitoring and follow-up visits and adhere to treatment recommendations. Multidisciplinary care involving hepatologists, addiction specialists, dietitians, and other healthcare professionals can help optimize management and improve outcomes.
Lifestyle adjustments, such as keeping a healthy diet, exercising within one’s capabilities, and avoiding hepatotoxic substances, are crucial in managing alcoholic cirrhosis.
The treatment of alcoholic cirrhosis focuses on several key aspects, including the following:
- Alcohol cessation: The most crucial step in managing alcoholic cirrhosis is abstinence from alcohol. This can help prevent further liver damage and may even allow for some improvement in liver function. It is essential to seek support from addiction treatment healthcare professionals, support groups, or addiction treatment programs to quit drinking and maintain sobriety successfully.
- Nutritional support: Malnutrition is common in individuals with alcoholic cirrhosis due to alcohol-related factors and impaired liver function. Nutritional counseling and dietary modifications may be recommended to ensure adequate nutrient intake.
- Medications: Several medications may be used to manage specific symptoms of alcoholic cirrhosis and complications. These can include:
- Diuretics: Diuretic drugs may be prescribed to reduce fluid retention (ascites) and swelling.
- Lactulose: Lactulose is commonly used to treat hepatic encephalopathy by reducing the buildup of toxic substances in the body.
- Beta-blockers: Beta-blocker medications may be prescribed to lower blood pressure in the portal vein and prevent the development or progression of varices.
- Ursodeoxycholic acid: This medication may manage cholestasis and improve liver function.
- Management of complications: Alcoholic cirrhosis can lead to various complications, such as ascites, hepatic encephalopathy, variceal bleeding, and infections. These complications require specific treatments, including therapeutic paracentesis (fluid removal), antibiotics, endoscopic procedures to address “Varices,” and other interventions as necessary.
- Liver transplantation: In advanced cases of alcoholic cirrhosis, liver transplantation may be considered when liver function has severely declined, and complications are severe. A transplant can provide a new, healthy liver. Still, eligibility and access to transplantation depend on various factors, including the severity of liver disease, overall health, and adherence to alcohol abstinence.
Treatment for Cirrhosis Caused by Alcohol
The most crucial step in managing alcohol-related cirrhosis is stopping alcohol altogether. This is crucial to prevent further liver damage and potentially improve liver function. It is essential to seek support from alcohol treatment healthcare professionals, support groups, or addiction treatment programs to quit drinking and maintain sobriety.
If you or someone you’re concerned with is struggling with alcoholic cirrhosis, immediate medical help is crucial. Contact We Level Up addiction treatment center for alcoholic cirrhosis prevention programs and treatment resources. Our addiction specialists can help you explore treatment options.
World-class, Accredited, 5-Star Reviewed, Effective Addiction & Mental Health Programs. Complete Behavioral Health Inpatient Rehab, Detox plus Co-occuring Disorders Therapy.
CALL(844) 597-1011End the Addiction Pain. End the Emotional Rollercoaster. Get Your Life Back. Start Drug, Alcohol & Dual Diagnosis Mental Health Treatment Now. Get Free No-obligation Guidance by Substance Abuse Specialists Who Understand Addiction & Mental Health Recovery & Know How to Help.
Top 10 What is Alcohol Cirrhosis? FAQs
-
Can you get cirrhosis of the liver without drinking alcohol?
Yes, cirrhosis of the liver can occur without alcohol consumption. While alcoholic cirrhosis is a common cause, several other causes of cirrhosis do not involve alcohol. Non alcoholic cirrhosis liver, also known as nonalcoholic steatohepatitis (NASH)-related cirrhosis, is a type of liver disease that occurs in people who do not consume excessive amounts of alcohol. It is closely associated with nonalcoholic fatty liver disease, described by fat accumulation in the liver.
-
How much alcohol causes cirrhosis?
The development of cirrhosis is strongly associated with long-term and excessive alcohol consumption. The quantity of alcohol that can lead to cirrhosis varies depending on individual factors such as genetic predisposition, overall health, and duration of alcohol abuse. However, there are generally accepted guidelines for safe alcohol consumption that can help minimize the risk of developing cirrhosis and other alcohol-related liver diseases.
-
What causes cirrhosis of the liver besides alcohol?
What causes cirrhosis of the liver other than alcohol? Cirrhosis of the liver can result from various factors other than alcohol consumption. Some common causes include viral hepatitis (such as hepatitis B and C), nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH), autoimmune hepatitis, genetic disorders (such as Wilson’s disease and hemochromatosis), chronic biliary obstruction, drug-induced liver injury, and certain metabolic conditions.
-
How much alcohol can you drink with cirrhosis?
It is generally advised that individuals with cirrhosis abstain entirely from drinking alcohol. Alcohol consumption, even in small quantities, can be detrimental to a compromised liver and may worsen the condition, increase the risk of complications, and accelerate the progression of cirrhosis. Therefore, it is strongly recommended to avoid any alcohol consumption if you have cirrhosis. It’s critical to consult with a healthcare professional for personalized advice and guidance regarding your specific condition.
-
What is the average age of alcoholic cirrhosis?
Alcoholic cirrhosis develops gradually over years or decades of excessive alcohol consumption. It is typically detected in individuals who have been drinking heavily for a prolonged period. Therefore, it is more commonly observed in middle-aged or older adults.
-
What is the stage 4 non alcoholic cirrhosis of the liver life expectancy?
Stage 4 cirrhosis, or decompensated cirrhosis, is characterized by severe liver damage and significant complications. At this stage, the liver’s ability to function correctly is significantly impaired, leading to various symptoms and health challenges. Generally, the prognosis for individuals with stage 4 nonalcoholic cirrhosis is poorer than earlier. Complications such as ascites (fluid buildup in the abdomen), hepatic encephalopathy (brain dysfunction due to liver dysfunction), variceal bleeding, and jaundice can significantly impact life expectancy.
-
What are the symptoms of alcoholic cirrhosis of liver without ascites?
Alcoholic cirrhosis of the liver is a late stage of liver disease caused by long-term, excessive alcohol consumption. It is characterized by replacing healthy liver tissue with scar tissue, which impairs the liver’s ability to function correctly. While the presence or absence of ascites (fluid accumulation in the abdominal cavity) can vary in individuals with alcoholic cirrhosis, several common signs of alcoholic cirrhosis are associated with this condition, even without ascites.
-
What are the symptoms of alcoholic cirrhosis of the liver with ascites?
Alcoholic liver cirrhosis can be accompanied by ascites, which accumulate fluid in the abdominal cavity. When ascites due to alcoholic cirrhosis are present, they can cause additional symptoms. Alcoholic cirrhosis with ascites can have significant implications for the overall prognosis and requires proper management, including dietary restrictions, diuretic medications, and potentially invasive procedures such as paracentesis to drain the accumulated fluid.
-
What is decompensated alcoholic cirrhosis?
Decompensated alcoholic cirrhosis is an advanced stage of liver disease where your liver can no longer act its essential functions adequately. It is described by the development of severe complications and the inability of the liver to maintain normal bodily functions. This stage of cirrhosis is considered a critical condition and requires immediate medical attention.
-
What is the difference between alcoholic hepatitis versus cirrhosis?
Alcoholic hepatitis and alcoholic cirrhosis are two distinct but related conditions that can occur as a result of chronic alcohol abuse and can coexist in some individuals. Alcoholic hepatitis and cirrhosis can coexist; in some cases, alcoholic hepatitis may progress to cirrhosis over time. Both conditions require medical attention and, most importantly, a cessation of alcohol consumption to prevent further liver damage and improve outcomes. Proper diagnosis and management by healthcare professionals are crucial for individuals with these conditions.
Alcoholism Treatment. Alcohol Use Disorder. Is Alcohol Addictive? Why Is Alcohol Addictive
Watch the below video about alcoholism treatment for further information. If you or someone you’re concerned with is struggling with alcohol use, get FREE addiction treatment insurance check – https://welevelup.com/rehab-insurance/
If you or a loved one is struggling with alcohol addiction or other substance use disorder(s), call for a FREE consultation 24/7 at (561) 678-0917
Alcoholism Treatment. Alcohol Use Disorder Video Transcript.
There are several names for alcoholism, such as alcohol addiction and alcohol dependency. It is now officially known as an alcohol use disorder. It happens when you drink so much alcohol that your body finally develops an addiction. When this occurs, alcohol takes on a major role in your life. Each technique used in alcoholism therapy for alcohol use disorder is intended to help you completely stop binge drinking.
Alcoholism is characterized as an alcohol use disorder. It is a pattern of binge drinking referred to as alcoholism. The likelihood of controlling your drinking, being concerned with alcohol, and continuing to consume alcohol even when it creates problems increases if you have excessive drinking issues. When you abruptly cut back or quit drinking, you may experience alcohol withdrawal symptoms or need to drink more to achieve the same impact.
Any alcohol usage that threatens your health or safety or results in other alcohol-related issues is considered unhealthy. A pattern of drinking where a man downs five or more drinks in two hours or where a woman downs at least four drinks in two hours is known as binge drinking. Significant threats to one’s health and safety result from binge drinking.
While some individuals may consume alcohol to the point where it becomes problematic, they are not physically dependent. Alcohol abuse used to be the term for this.
Experience Transformative Recovery at We Level Up Treatment Centers.
See our authentic success stories. Get inspired. Get the help you deserve.
Start a New Life
Begin with a free call to an addiction & behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up Treatment Center Network delivers recovery programs that vary by each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- World-class Amenities
- Licensed & Accredited
- Renowned w/ 100s 5-Star Reviews
We’ll Call You
Search We Level Up Alcoholic Cirrhosis, Detox, Mental Health Topics & Resources
Sources
[1] Newman RK, Stobart Gallagher MA, Gomez AE. Alcohol Withdrawal. [Updated 2022 Aug 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441882/
[2] Alcohol Facts and Statistics – National Institute on Alcohol Abuse and Alcoholism (NIAAA)
[3] Nehring SM, Freeman AM. Alcohol Use Disorder. [Updated 2022 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK436003/
[4] Alozai Uu, Sharma S. Drug and Alcohol Use. [Updated 2022 Jun 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513263/
[5] Alcohol use disorder – Available from: https://medlineplus.gov/download/genetics/condition/alcohol-use-disorder.pdf
[6] Huebner RB, Kantor LW. Advances in alcoholism treatment. Alcohol Res Health. 2011;33(4):295-9. PMID: 23580014; PMCID: PMC3860532.
[7] Center for Substance Abuse Treatment. A Guide to Substance Abuse Services for Primary Care Clinicians. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 1997. (Treatment Improvement Protocol (TIP) Series, No. 24.) Chapter 5—Specialized Substance Abuse Treatment Programs. Available from: https://www.ncbi.nlm.nih.gov/books/NBK64815/
[8] LaHood AJ, Kok SJ. Ethanol Toxicity. [Updated 2023 Mar 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557381/
[9] Alcohol’s Effects on Health – National Institute on Alcohol Abuse and Alcoholism (NIAAA)
[10] Alcohol’s Effect on Health: NIAAA brochures and fact sheets – National Institute on Alcohol Abuse and Alcoholism (NIAAA)


