What are Benzodiazepines Used For? What are Benzodiazepines Drugs?
What do benzodiazepines do? Benzodiazepines, also known as “benzos,” are a class of drugs used to treat various conditions. Conditions commonly treated with benzos include insomnia, anxiety, sleep disorders, and even alcohol withdrawal. These substances act on the GABA receptors in the brain as they produce a very calming effect. Unfortunately, benzo addiction can develop in as little as a month. High-risk patients or those with unstable medical conditions or a significant seizure history may benefit from admission to an inpatient service for benzodiazepine detox to manage the risks of benzodiazepines withdrawal symptoms safely. [1]
Gamma-aminobutyric acid or GABA is a naturally occurring amino acid that works as a neurotransmitter in your brain.***
Short-Term Adverse Effects of Benzodiazepines
- Drowsiness
- Confusion
- Dizziness
- Trembling
- Impaired Coordination
- Vision Problems
- Grogginess
- Feelings of Depression
- Headache
Long Term Effects of Benzodiazepines When Misused or Abused
- Possible Dementia
- Physical Dependence
- Overdose
Benzodiazepine Addiction & Dependence
Benzodiazepine dependence is different from benzo addiction because addiction occurs only in some people. When you take benzos for multiple days or weeks, the brain adapts to the presence of the drugs. As a result, you may start to depend on the drugs to function. Benzo dependency is the state of relying on benzo to feel natural.
As drug dependency amplifies, the brain begins to need larger doses to feel similar effects. Requiring more significant amounts of a substance is an adaptation called tolerance. For example, when someone dependent on benzo stops taking the drug, they experience benzo withdrawal symptoms as the risks of benzos. [3]
Benzodiazepines Mechanism of Action (Benzodiazepines MOA)
Benzos are a class of drugs that act upon benzodiazepine receptors (BZ-R) in the central nervous system (CNS). Benzos are commonly administered via the oral and intravenous routes. They may also be administered rectally, intranasally, and intramuscularly, as protocol/patient presentation dictates.
Benzos are especially important in the cessation of seizure activity, as 1% to 2% of emergency department visits annually in the United States are for seizures. Indications for benzodiazepine administration include but are not limited to anxiety disorders, insomnia, acute status epilepticus, induction of amnesia, spastic disorders, seizure disorders, and agitation. How do benzodiazepines work? To simplify the benzodiazepine mechanism of action (benzodiazepine MOA):
- Benzos bind to “benzodiazepine receptors” located between alpha and gamma subunits of GABA-A receptor/channel complexes
- GABA needs to be present for benzodiazepine effects to be detectable
- Benzodiazepines increase the frequency of the chloride ion channel opening, thereby increasing the inhibitory effect of GABA on neuronal excitability
- MOA benzodiazepine effects are especially pronounced in the limbic system, thalamus & hypothalamus
FDA-Approved List of Benzodiazepines
The most common benzodiazepines are the prescription drugs Valium®, Xanax®, Halcion®, Ativan®, and Klonopin®.
As we discussed further the uses of benzos, you will be able to understand how the following list of benzodiazepine drugs are beneficial and have their own risks.
- Alprazolam (Xanax) – Prescribed for anxiety/panic disorders
- Chlordiazepoxide – Primarily indicated for alcohol withdrawal syndrome
- Clobazam – Indicated for seizures
- Clonazepam (Klonopin) – For panic disorder and certain types of seizures
- Clorazepate – Short-term medication for anxiety disorders
- Diazepam (Valium) – Alcohol withdrawal management and seizures medication
- Estazolam (Prosom) – Treament for insomnia
- Flurazepam – Insomnia medication
- Lorazepam (Ativan) – Treatment for anxiety disorders
- Midazolam – Convulsive status epilepticus and procedural sedation
- Oxazepam – Anxiety disorders and alcohol withdrawal syndrome treatment
- Quazepam – Indicated mainly for chronic insomnia in adults
- Temazepam – Sleep maintenance insomnia
- Triazolam – Primarily indicated for sleep-onset insomnia
- Remimazolam – Procedural sedation for adults
How Do Benzos Work? Benzodiazepine Uses
Benzos are only legally available through prescription. Many users maintain their drug supply by getting prescriptions from several doctors, forging prescriptions, or buying them illicitly. Alprazolam (Xanax) and clonazepam (Klonopin) are the two most frequently encountered benzos on the illicit market.
Benzos are controlled in Schedule IV of the Controlled Substances Act. [2] Schedule IV drugs, substances, or chemicals are defined as drugs with a low potential for abuse and a low risk of dependence. However, this doesn’t mean that it is in any way less dangerous and addictive. Some benzodiazepines examples of Schedule IV drugs are Xanax, Valium, Ativan, and Klonopin.
Types of Benzodiazepines
There are three benzodiazepines types: long-acting, intermediate-acting, and short-acting. Short acting benzodiazepines produce more severe withdrawal symptoms and can be more addictive than long acting benzodiazepines.
The least addictive benzodiazepines are the long-acting benzos such as chlordiazepoxide (intermediate onset), flurazepam (slow onset), and prazepam (slowest onset).
Skip To:
Learn More:
Benzodiazepines Classification & Drug Facts
Benzodiazepines Meaning
what is benzodiazepines drug class? Benzodiazepine drugs (BEN-zoh-dy-A-zeh-peen)(“Benzodiazepinas” in Spanish) are a group of depressant drugs. Common benzodiazepines are prescribed drugs in outpatient and hospitalized patients. Benzodiazepines medications are effective for sedation and anxiolysis; they also have the potential to cause harm.
Benzos are only legally available through prescription.
All healthcare professionals, including clinicians (MD, DO, NP, PA) who prescribe these benzodiazepine medications, must be fully aware of the drug’s adverse effects, misuse, abuse, and potential to develop physical dependence.
Barbiturates vs Benzodiazepines
In terms of benzodiazepines vs barbiturates, the fundamental distinction between the two is that benzodiazepines do not directly excite the GABA receptor; instead, they just increase the efficiency of GABA receptors. Benzodiazepines effects continue to be relaxing, although they do not have the same depressing impact on the central nervous system as barbiturates.
For most of these clinical purposes, benzos and the newer non-benzodiazepine hypnotics are currently favored over barbiturates because they have a wider therapeutic index, tolerance builds more slowly, and their abuse potential is lower than that of barbiturates.
Common Types of Benzodiazepines
| Generic Name | Brand Name | Onset of Effect | Dose Equivalents (mg) |
|---|---|---|---|
| alprazolam | Xanax | fast/intermediate | 0.5 |
| chlordiazepoxide | Librium | intermediate | 25 |
| clonazepam | Klonopin | intermediate | 0.5 |
| clorazepate | Tranxene | intermediate | 15 |
| diazepam | Valium | fast | 10 |
| estazolam | ProSom | slow | 2 |
| flunitrazepam | Rohypnol | fast | 1 |
| flurazepam | Dalmane | fast | 20 |
| lorazepam | Ativan | fast | 1 |
| midazolam | Versed | fast | 15 (IV) |
| oxazepam | Serax | slow | 20 |
| quazepam | Doral | slow | 20 |
| temazepam | Restoril | intermediate | 20 |
| triazolam | Halcion | fast | 0.5 |
Benzodiazepines Drug Facts Sheet by the DEA Publicly Made Available for Substance Use Disorder Awareness
Benzodiazepines (sometimes called “benzos”) work to calm or sedate a person, by raising the level of the inhibitory neurotransmitter GABA in the brain. Common benzodiazepines include diazepam (Valium), alprazolam (Xanax), lorazepam (Ativan), and clonazepam (Klonopin), among others.
In 2020, 16% of overdose deaths involving opioids also involved benzodiazepines, a type of prescription sedative commonly prescribed for anxiety or to help with insomnia. [4]
According to the National Institute on Drug Abuse, every day, nearly 200 Americans die after overdosing on opioids. Combining opioids and benzodiazepines can increase risk of overdose because both types of drugs can cause sedation and suppress breathing—the cause of overdose fatality—in addition to impairing cognitive functions. Research shows that people who use opioids and benzodiazepines concurrently are at higher risk of visiting the emergency department, being admitted to a hospital for a drug-related emergency, and dying of drug overdose.

Get Your Life Back
Find Hope & Recovery. Get Safe Comfortable Detox, Addiction Rehab & Dual Diagnosis High-Quality Care.
Hotline(844) 597-1011Benzodiazepines Addiction Statistics
While benzodiazepines are important therapies for many Americans, they are also commonly abused and misused, often together with opioid pain relievers and other medicines, alcohol, and illicit drugs. Benzodiazepines, such as Xanax, Ativan, and other benzo sedatives, are often used for the short-term treatment of anxiety and insomnia. While benzodiazepine use is highly prevalent among U.S. adults, public health experts have not known what proportion of benzodiazepine users misuse them or meet the criteria for benzodiazepine use disorders. Nevertheless, benzodiazepine use was associated with emergency room visits, mental disorders, suicidal ideation, and substance use.
Physical dependence can occur when benzodiazepines are taken steadily for several days to weeks. Patients who have been taking a benzodiazepine for weeks or months can have withdrawal signs and symptoms when the medicine is discontinued abruptly or continued in lower doses to avoid withdrawal. Stopping benzodiazepines abruptly or reducing the dosage too quickly can result in acute withdrawal reactions, including seizures, which can be life-threatening. Prior to stopping benzodiazepines, patients should talk to their healthcare provider to develop a plan for slowly tapering the medication.
20%
Benzodiazepine use among U.S. adults is high and misuse accounted for nearly 20% of use overall.
Source: NCBI
30.5 Million
12.5% of adults in the United States use benzos. This equates to about 30.5 million people.
Source: NCBI
≥65
Benzodiazepine use among adults 50–64 has now exceeded use by those ≥65.
Source: NCBI
Different Examples of Benzodiazepines
What is benzodiazepine used for? Benzodiazepines provide short-term relief from distressing feelings but can become a problem in the long run. You can become dependent on the medication and end up feeling like you cannot face stressful situations without it. If you take benzos for a long period of time you can become physically dependent. This means you would go into “withdrawal” without the medication. In withdrawal, cravings can be constant and intense. At this point, it is hard to stop taking the medication.
Efforts to obtain the medication to stop the withdrawal symptoms can get in the way of other things like work and family. It can also be dangerous if done suddenly, without the help of a health care provider. Doctors often prescribe benzos to treat anxiety, seizures, and insomnia. Here are some of the known benzodiazepine examples:
Alprazolam (Xanax, Kalma, Xanax® XR)
- Alprazolam is used to treat anxiety disorders and panic disorder (sudden, unexpected attacks of extreme fear and worry about these attacks). Is Xanax a benzodiazepines? Yes. Alprazolam is in a class of medications called benzos. It works by decreasing abnormal excitement in the brain.
- Alprazolam, sold under the brand name Xanax, may cause physical dependence (a condition in which unpleasant physical symptoms occur if a medication is suddenly stopped or taken in smaller doses), especially if you take it for several days to several weeks. [4]
- Alprazolam (Xanax® XR, Xanax®, Kalma®) is a Triazolobenzodiazepine used in panic disorder and other anxiety states. Benzodiazepine Xanax is significantly more toxic than other benzos. The increased prescription of alprazolam to groups with an increased risk of deliberate self-poisoning is concerning and needs review. [5]
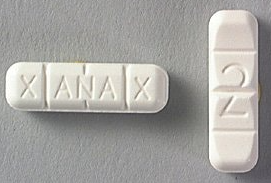
How Much Xanax Does It Take To Overdose?
It’s possible to overdose on Xanax, especially if you take Xanax with other drugs or medications. The amount that could potentially lead to an overdose varies widely from person to person. It depends on many factors, including:
- How your body metabolizes the medication
- Your weight
- Your age
- If you have any preexisting conditions, like a heart, kidney, or liver condition
- If you took it with alcohol or other drugs (including antidepressants)
Mixing Xanax and alcohol can also be fatal. Xanax is in a class of drugs known as benzodiazepines. These drugs work by boosting the activity of a chemical called gamma-aminobutyric acid (GABA) in the brain. GABA helps calm the nerves by inducing feelings of relaxation. Most severe or fatal overdoses happen when Xanax is taken with other drugs — especially opioid pain medications — or alcohol.
If you’re taking Xanax dosages, be sure to tell your doctor about any other medications you’re taking. They may recommend an alternative medication.
Oxazepam (Serax, Alepam, Murelax)
- Oxazepam is used to relieve anxiety, including anxiety caused by alcohol withdrawal (symptoms that may develop in people who stop drinking alcohol after drinking large amounts for a long time). Oxazepam is in a class of medications called benzos. It works by slowing activity in the brain to allow for relaxation.
- Oxazepam may cause physical dependence (a condition in which unpleasant physical symptoms occur if a medication is suddenly stopped or taken in smaller doses), especially if you take it for several days to several weeks. [6]
Temazepam (Restoril, Normison, Temaze, Temtabs, Euhypnos)
- Temazepam is used on a short-term basis to treat insomnia (difficulty falling asleep or staying asleep). Temazepam is in a class of medications called benzos. It works by slowing activity in the brain to allow sleep. Temazepam side effects may also be habit-forming. [7]
Although Temazepam is a scheduled IV drug, you should be very careful taking this drug. This drug has black box warnings. The following are the most serious warnings from the Food and Drug Administration (FDA):
- Suicidal thinking and behavior warning: This drug can increase the risk of suicidal thinking and behavior in children, adolescents, and young adults. This is more likely to happen during the first few months of treatment with this drug. When you or your child first start taking this drug, your doctor and family should watch closely. They should look for changes in behavior or worsening signs of depression.
- Dangerous effects with opioid use: Using this drug with opioid drugs, such as hydrocodone, or codeine, can cause dangerous effects. Your risk is higher if you take high doses of either drug and take them for a long time. Call your doctor or 911 right away if you or someone you’re caring for has symptoms of unusual dizziness or lightheadedness, extreme sleepiness, slowed or difficult breathing, or unresponsiveness. These symptoms can lead to coma and even death.
- Physical dependence and withdrawal reactions: Taking this medication for several days to weeks can cause physical dependence and withdrawal reactions. Do not suddenly stop taking this medication without talking with your doctor. If you suddenly stop taking this medication, you may have withdrawal symptoms, which can be life-threatening.
- Misuse and addiction: Taking this medication can lead to misuse and addiction. This can increase your risk of overdose and death.
Flunitrazepam (Rohypnol)
Flunitrazepam is a benzodiazepine with pharmacologic actions similar to those of diazepam that can cause anterograde amnesia. Some reports indicate that it is used as a date rape drug and suggest that it may precipitate violent behavior. The United States Government has banned the importation of this drug.
- It is not approved for medical use in the United States. Used by cocaine abusers to relieve side effects, and is also used as a date rape drug. [8]
- Street Names are “Circles, Date Rape Drug, Forget Pill, Forget-Me Pill, La Rocha, Lunch Money, Mexican Valium, Mind Eraser, Pingus, R2, Reynolds, Rib, Roach, Roach 2, Roaches, Roachies, Roapies, Rochas Dos, Roofies, Rope, Rophies, Row-Shay, Ruffies, Trip-and-Fall, Wolfies”

Nitrazepam (Mogadon, Alodorm)
- Nitrazepam is a DEA Schedule IV controlled substance. Substances in the DEA Schedule IV have a low potential for abuse relative to substances in Schedule III.
- It is used as a hypnotic for the short-term management of insomnia and for the treatment of epileptic spasms in infants (West’s syndrome). It has a role as an anticonvulsant, an antispasmodic drug, a GABA modulator, a sedative and a drug metabolite. It is a 1,4-benzodiazepine and a C-nitro compound. [9]
Clonazepam (Rivotril, Paxam, Klonopin)
- Antiepileptic drugs have been used in pain management since the 1960s; some have shown efficacy in treating different neuropathic pain conditions. Clonazepam, a benzodiazepine, is an established antiepileptic drug, but its place in the treatment of neuropathic pain is unclear.
- Dependence and tolerance may occur with prolonged use. [10]
First-class Facilities & Amenities
World-class High-Quality Addiction & Mental Health Rehabilitation Treatment
Rehab Centers TourRenowned Addiction Centers. Serene Private Facilities. Inpatient rehab programs vary.
Addiction Helpline(844) 597-1011Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Success Stories Across Our Network
- Low Patient to Therapist Ratio
- Onsite Medical Detox Center
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Personal Development Events
Lorazepam (Ativan)
Ativan is used to relieve anxiety. Ativan is in a class of medications called benzos. It works by slowing activity in the brain to allow for relaxation. Ativan is also used to treat irritable bowel syndrome, epilepsy, insomnia, nausea, and vomiting from cancer treatment and to control agitation caused by alcohol withdrawal.
Physiological dependence on benzodiazepines can occur following prolonged treatment with therapeutic doses, but it is not clear what proportion of patients are likely to experience withdrawal syndrome. It is also unknown to what extent the risk of physiological dependence is dependent upon a minimum duration of exposure or dosage of these drugs. Withdrawal phenomena appear to be more severe following withdrawal from high doses of short-acting benzodiazepines. Dependence on alcohol or other sedatives may increase the risk of benzodiazepine dependence.
- Is lorazepam a benzodiazepine? Yes. Lorazepam is a benzodiazepine medication commonly used as the sedative and anxiolytic of choice in the inpatient setting owing to its fast (1 to 3 minute) onset of action when administered intravenously. [11]
- Serious adverse effects of lorazepam include dependence and Ativan abuse.
Diazepam (Valium, Antenex, Ducene, Ranzepan, Valpam)
Certain prescription drugs are more addictive than others, such as Valium. Most addictive medicines work by flooding your brain’s reward system with dopamine. This produces a pleasurable “high” that may entice you to use the substance again. You may grow dependent on the drug to feel “good” or “normal” over time, and you may also build a tolerance to the substance. This may cause you to take higher dosages.
you should know that your mental health may change in unexpected ways and you may become suicidal (thinking about harming or killing yourself or planning or trying to do so) while you are taking diazepam for the treatment of epilepsy. A small number of adults and children 5 years of age and older (about 1 in 500 people) who took anticonvulsants such as diazepam to treat various conditions during clinical studies became suicidal during their treatment.
Some of these people developed suicidal thoughts and behavior as early as one week after they started taking the medication. There is a risk that you may experience changes in your mental health if you take an anticonvulsant medication such as diazepam, but there may also be a risk that you will experience changes in your mental health if your condition is not treated. You and your doctor will decide whether the risks of taking an anticonvulsant medication are greater than the risks of not taking the medication.
- Diazepam is a DEA Schedule IV controlled substance. Substances in the DEA Schedule IV have a low potential for abuse relative to substances in Schedule III.
- Diazepam is a benzodiazepine derivative with anti-anxiety, sedative, hypnotic and anticonvulsant properties. Diazepam potentiates the inhibitory activities of gamma-aminobutyric acid (GABA) by binding to the GABA receptor, located in the limbic system and the hypothalamus. [12]
Benzodiazepine Equivalency Table & Benzodiazepine Comparison Chart
Below is the benzodiazepines list in order of strength. Many benzos have long half-lives and these drugs undergo various types of hepatic metabolism (the type of benzodiazepine metabolism and rates depend on the individual drug). Benzodiazepines contraindications include a known case of angle-closure glaucoma. Benzos have muscle relaxant effects that can affect the function of the sphincter pupillae muscle of the iris. Benzos are also contraindicated in patients with prior hypersensitivity reactions. Anaphylaxis and angioedema have been reported. Remimazolam is contraindicated in patients with a history of hypersensitivity reaction to dextran 40.
Box Warning: Concomitant use of benzos with opioids can lead to sedation, severe respiratory depression, coma, and death. Avoid combination.
Generic Benzodiazepine List of Drugs Name
Onset (Hours)
Example of Benzodiazepines Action Duration
Benzodiazepine Half Life Chart (Hours)
Potency Benzodiazepine Equivalency Chart
Benzodiazepine Equivalent Chart for Doses (mg) Benzodiazepine Conversion
Flurazepam
Chlordiazepoxide
Diazepam
Clorazepate
Clonazepam
Temazepam
Lorazepam
Oxazepam
Alprazolam
Triazolam
1
1.5
1
1
1
0.5
2
3
1
0.5
Long
Long
Long
Long
Long
Intermediate
Intermediate
Short
Short
Short
*40-250
*36-200
*36-200
*36-201
18-50
8-22
10-20
4-15
6-12
2-5
Low
Low
Low
Low
High
Low
High
Low
High
High
15-30
10-25
5-10
7.5-15
0.25-0.5
30
1
15-20
0.5
0.25-0.5
Benzodiazepines for Anxiety
Benzos are among the most commonly prescribed drugs for anxiety disorders. While they are indicated as an adjunctive medication for short-term use according to clinical practice guidelines, previous studies have shown patterns of long-term use of benzos, which is problematic due to side effects, dependence, and the potential for substance abuse.
While benzos have also demonstrated efficacy for some anxiety disorders treatment, they are generally recommended in CPGs (clinical practice guidelines) as adjunctive short-term options, preferably with regular dosing, either to help relieve patients with acute anxiety and agitation or pending a response to antidepressants. With their rapid anxiolytic and sedative/hypnotic effects, benzos provide effective short-term relief for insomnia and anxiety.
Despite knowledge of the risks of the long-term use of benzos, this remains a pervasive problem. Clinicians need to be mindful of patterns and risk factors leading to the long-term use of benzodiazepines in patients with anxiety disorders. Are you searching for “benzodiazepine friendly doctors near me?” How to get a doctor to prescribe benzodiazepines for anxiety? Contact an accredited mental health treatment center that is aware of the risks of medications and substance abuse. It is best to get help with treatment facilities that offer dual diagnosis treatment, offering simultaneous treatment for substance use and mental health problems.
Alternatives to Benzodiazepines for Anxiety
Anxiety disorders are among the most prevalent mental disorders experienced in the general population. Evidence-based treatment options for anxiety disorders comprise psychological and pharmacological treatments. According to clinical practice guidelines (CPGs), selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs) are generally first-line pharmacological treatments for anxiety disorders since they present advantageous safety and tolerability profiles.
The following medications are all options for anxiety that are alternatives to addictive benzodiazepines. Drugs like Xanax that aren’t addictive are SSRIs, SNRIs, buspirone, beta-blockers, pregabalin, gabapentin, hydroxyzine, Panax, and diphenhydramine.
Benzodiazepines for Seizures
Benzodiazepines are also used to relax muscles and prevent seizures. They increase the effect of a chemical in the brain called GABA, which is a neurotransmitter (a substance that nerves use to send messages to one another). This causes brain activity to slow down. Benzodiazepines are a type of CNS depressant.
Benzodiazepines remain important agents in the management of epilepsy. They are drugs of first choice for status epilepticus and seizures associated with post-anoxic insult and are also frequently used in the treatment of febrile, acute repetitive, and alcohol withdrawal seizures. Clinical advantages of these drugs include rapid onset of action, high efficacy rates, and minimal toxicity. Benzodiazepines are used in a variety of clinical situations because they have a broad spectrum of clinical activity and can be administered via several routes. Potential shortcomings of benzos include tolerance, withdrawal symptoms, adverse events, such as cognitive impairment and sedation, and drug interactions.

Benzodiazepines Side Effects
Do benzodiazepines cause respiratory depression? Unfortunately, yes. benzodiazepines (and benzodiazepine-like drugs) and opioid medicines (opioids) can both cause respiratory depression; when used together, additive effects on the central nervous system increase the risks of sedation, respiratory depression, coma, and death.
Common side effects of benzodiazepines administration include, but are not limited to:
- Respiratory depression
- Respiratory arrest
- Drowsiness
- Confusion
- Headache
- Syncope
- Nausea/vomiting
- Diarrhea
- Tremor
There is no accurate, generally accepted prescription guideline for benzodiazepines. These medications are prescribed at about 66 million doctors’ appointments a year in the U.S., according to a report by the U.S. National Center for Health Statistics. A recent study showed that benzodiazepine prescribing had nearly doubled from 2003 through 2015 for ambulatory care visits.
For every 100 adults that visit an office-based doctor over the course of a year, 27 visits will result in a prescription for a benzodiazepine. Opioid overdose deaths that included benzos increased an astounding 1082% between 1999 and 2020, and 30% of overdose deaths involve BZD use. The overdose mortality rate involving benzodiazepines for women between the ages of 30 and 64 has increased by 830 percent between 1996 and 2017. Four-fifths of those prescribed benzos indicate use for more than six months, far beyond the “short-term” use recommendation of the FDA.
Drug-Drug Interactions
- Benzodiazepines may interact with ethanol, other benzodiazepines, and sedatives such as barbiturates, resulting in increased respiratory depression via a synergistic effect. Therefore, concomitant administration of benzodiazepines with patients under the influence of the preceding drugs should be carefully performed, with respiratory monitoring in place.
- Lorazepam and oxazepam are metabolized by UGT (Uridine diphosphate glucuronosyltransferases). Inducers of UGT, such as carbamazepine, phenobarbital, phenytoin, and rifampin, may induce the metabolism and decrease the efficacy.
- Excessive sedation can result from concurrent administration of benzodiazepine-like midazolam, triazolam, alprazolam, or diazepam administered with strong CYP3A4 inhibitors like itraconazole, ketoconazole, grapefruit juice, clarithromycin, nefazodone, ritonavir. Avoid concurrent administration.
What Can Show Up as Benzodiazepine in a Urine Test?
False-positive screens for drugs of abuse can potentially hamper diagnosis and treatment. If a patient’s clinical presentation is prematurely ascribed to a substance disorder, a medical workup may be less aggressively pursued, potentially forestalling the correct diagnosis and early treatment. Moreover, when patients are misdiagnosed with a substance-related disorder based on false test results—despite their truthful denial of substance use—the crucial therapeutic alliance may be damaged. Such potential consequences underscore the importance of knowing the validity of screening tests for drugs of abuse.
- False Negative Benzodiazepines Urine Test – False-negative benzodiazepines urine test can arise when the drug concentration in the urine is less than the amount specified by the laboratory performing the test. False negatives may be affected by diluted urine, the amount of time between drug consumption and testing, and the amount of substance taken.
- False Positive Drug Test Benzodiazepines – False-positive results might be more common than many clinicians realize. If you use OTC NSAIDs, your urine test may come up positive for barbiturates (a form of sedative) or THC. Oxaprozin (Daypro), another NSAID, can be used to relieve arthritic pain. Consuming oxaprozin may cause a false positive benzodiazepine test. Barbiturates are not benzos. Barbiturates are a group of drugs in the class of drugs known as sedative-hypnotics. Unfortunately, both benzodiazepines and barbiturates drug classes can be highly addictive.
Benzodiazepines and Alcohol
Concomitant excessive consumption of alcohol and benzodiazepines use is associated with adverse health outcomes. When benzodiazepines and alcohol are used concurrently, their sedative effects significantly increase the risk of adverse events, including fatal overdose. Long-term consequences of combined benzodiazepine and alcohol use include cardiovascular, gastrointestinal, hepatic, kidney, and neurologic injury and exacerbation of psychiatric conditions. Despite this drug-drug interaction, benzodiazepines have the largest and the best evidence base in the treatment of alcohol withdrawal and are considered the gold standard.
Benzodiazepines for Alcohol Withdrawal
Alcohol withdrawal syndrome ranges from mild to severe. The severe complicated alcohol withdrawal may present with hallucinations, seizures, or delirium tremens. Over the years, the treatment for alcohol detoxification has evolved from the use of a gradual weaning schedule of alcohol itself to the use of benzodiazepines and newer miscellaneous drugs.
Benzodiazepines are safe, effective, and the preferred treatment for alcohol withdrawal syndrome. The best-studied benzodiazepines for alcohol withdrawal treatment are diazepam, chlordiazepoxide, and lorazepam. The three goals of drug and alcohol detoxification as described by the American Society of Addiction Medicine (ASAM) are as follows:
- “To provide a safe withdrawal from the drug(s) of dependence and enable the patient to become drug-free”.
- “To provide a withdrawal that is humane and thus protects the patient’s dignity”.
- “To prepare the patient for ongoing treatment of his or her dependence on alcohol or other drugs.”
Alcohol withdrawal syndrome results in people who are dependent on alcohol and either stop drinking or reduce their alcohol consumption. This results from a shift in the neurotransmitter levels in the brain, from GABA inhibition to glutaminergic stimulation. The symptoms are generally mild to moderate and resolve within a few days. However, severe forms of alcohol withdrawal syndrome may be associated with generalized seizures, hallucinations, and delirium tremens, which can be fatal.
Oral benzodiazepines are the best-studied and most effective drugs for preventing severe alcohol withdrawal syndrome, particularly the risk of seizures and delirium. For delirium tremens and withdrawal seizures, treatment with high-dose benzodiazepines (parenteral or oral) is recommended in the ICU setup.
World-class, Accredited, 5-Star Reviewed, Effective Addiction & Mental Health Programs. Complete Behavioral Health Inpatient Rehab, Detox plus Co-occuring Disorders Therapy.
CALL(844) 597-1011End the Addiction Pain. End the Emotional Rollercoaster. Get Your Life Back. Start Drug, Alcohol & Dual Diagnosis Mental Health Treatment Now. Get Free No-obligation Guidance by Substance Abuse Specialists Who Understand Addiction & Mental Health Recovery & Know How to Help.
Are Benzodiazepines Addictive? Benzodiazepines Uses & Abuse
Like other drug addiction effects, benzos cause a dopamine discharge. Dopamine is a chemical that contributes to how we feel pleasure. Over time, these drugs alter the way the brain releases dopamine. This affects the way people feel euphoria or happiness from all activities. As a result, people addicted to benzos can sometimes feel happy unless they take large doses of the drugs.
Addiction also alters the motivation system in the brain. The brain correlates the substances with happiness and causes cravings that drive the person to take the drugs, and withdrawal is another part of benzodiazepines dependency and addiction. People who attempt to discontinue the drugs on their own are seldom able to make it through withdrawal. Instead, the symptoms are usually so painful that people return to the benzos for relief.
Benzos can also be addictive because they momentarily alleviate specific mental health issues. For example, some people self-medicate with benzos to mitigate anxiety or sleep difficulties. The drugs can temporarily manage these illnesses, but long-term use can make people think they have to have the drugs to feel less troubled.
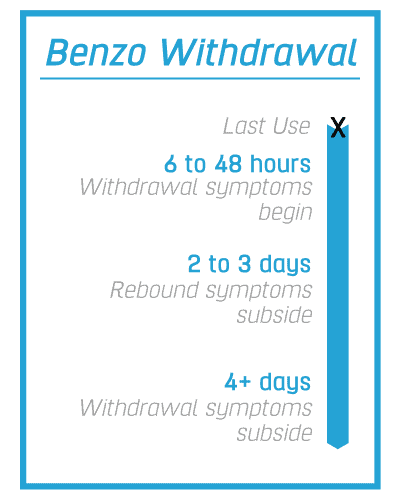
Benzo Withdrawal Timeline
If benzodiazepines are taken for two weeks or more, it is not suggested that the person discontinue this medication abruptly. Rather, benzodiazepines should be progressively decreased over a long period of time. Tapering off dose by 50% the first 2-4 weeks then maintain on that dose for 1-2 months then reduce dose by 25% every two weeks.
Rebound Anxiety & Insomnia
Withdrawal from normal dosage benzodiazepine treatment can result in a number of symptomatic patterns. The most common is a short-lived “rebound” anxiety and insomnia, coming on within 1-4 days of discontinuation, depending on the half-life of the particular drug.
Withdrawal Syndrome
The second pattern is the full-blown withdrawal syndrome, usually lasting 10-14 days; finally, a third pattern may represent the return of anxiety symptoms which then persist until some form of treatment is instituted.
Physiological dependence on benzodiazepines can occur following prolonged treatment with therapeutic doses, but it is not clear what proportion of patients are likely to experience withdrawal syndrome. It is also unknown to what extent the risk of physiological dependence is dependent upon a minimum duration of exposure or dosage of these drugs.
What can make benzodiazepines withdrawal worst?
Withdrawal phenomena appear to be more severe following withdrawal from high doses or short-acting benzodiazepines. Dependence on alcohol or other sedatives may increase the risk of benzodiazepine dependence, but it has proved difficult to demonstrate unequivocally differences in the relative abuse potential of individual benzodiazepines.
Benzo withdrawal symptoms will differ depending on how the detox process is administered. For instance, in a professional detox center where the client is weaned off properly, symptoms include feeling sleepy and depressed and sweating and chills.
Benzodiazepine Withdrawal Symptoms
To withdraw from benzodiazepines is difficult for many. Physiological dependence on benzodiazepines is accompanied by a withdrawal syndrome which is typically characterized by:
- Sleep disturbance
- Irritability
- Increased tension and anxiety
- Panic attacks
- Hand tremors
- Sweating
- Difficulty in concentration
- Nausea
- Some weight loss
- Palpitations
- Headache
- Muscular pain and stiffness and a host of perceptual changes
Benzodiazepine Withdrawal Syndrome
Benzodiazepine withdrawal becomes much more severe and fatal, most especially without medical supervision. You may develop Benzodiazepine withdrawal syndrome which could cause more painful effects on your body and mind.
General
- Headache
- Palpitations
- Sweating
- Tremor
- Muscle pain, stiffness, and aches (limbs, back, neck, jaw)
- Neurological
- Dizziness
- Paraesthesia or shooting pains in the neck and spine
- Visual disturbances (blurred vision, diplopia, photophobia, image lags behind eye movements)
- Tinnitus
- Faintness and dizziness, a sense of instability
- Confusion, disorientation (may be intermittent): A common cause of disorder in older patients
- Delirium (in the absence of autonomic hyperactivity): Particularly in older patients
- Delusions, paranoia
- Hallucinations (visual, auditory)
- Grand mal seizures 1–12 days after discontinuing benzodiazepines
Gastrointestinal
- Nausea
- Anorexia
- Diarrhea (may resemble irritable bowel syndrome)
Psychological
- Rebound insomnia, nightmares
- Anxiety, panic attacks
- Irritability, restlessness, agitation
- Poor memory and concentration
- Perceptual distortions – sensory hypersensitivity (light, sound, touch, taste), abnormal sensations (e.g., ‘cotton wool’ sensations)
- Metallic taste
- Distortions of body image
- Feelings of unreality, depersonalization, derealization
- Depression
- Benzo addiction. Even when the drugs are taken responsibly within a doctor’s recommended “safe window” of use, Benzodiazepine addiction can develop
How Long Does It Take To Develop Benzo Addiction?
You should only be prescribed benzos for the shortest amount of time possible. Taking benzos regularly for a few weeks or more can lead to addiction. Doctors recommend that you only take them for 2-4 weeks. Intermittent use may help to avoid addiction.
One of the most significant risks of benzos and the reason to get into a benzo addiction treatment program is likely overdosing. With the capacity to develop a tolerance, the longer someone takes benzos, the greater dosage they will need to take to reach the desired effect. Hence, the greater the risk of overdosing. Moreover, sedative benzos cause breathing to slow. In turn, less oxygen is directed through the lungs to the brain and the rest of the body. Finally, once you take a larger dose, breathing delays to the point of being fatal.
A benzodiazepine overdose can lead to:
- Extreme sedation or drowsiness
- A very low breathing rate
- Confusion and difficulty thinking
- Slurred speech
- Loss of muscle control
- Coma
Anyone who shows signs of a drug overdose or an adverse reaction after taking benzos will need emergency medical help.
It can be fatal if a person:
- Uses drugs with alcohol or opioids
- Is older and takes too much of the drug
- Is taking other drugs, and the effects build up in their body
Benzodiazepine Overdose Symptoms
Patients with benzodiazepine toxicity will primarily present with central nervous system depression ranging from mild drowsiness to a coma-like, stuporous state. The classic presentation of an isolated benzodiazepine overdose consists of CNS depression with normal vital signs. Cardiac-related effects and fatalities are rare in pure benzodiazepine toxicities.
Life-threatening respiratory depression can be seen with large oral ingestions with or without any substance that is congested simultaneously. Iatrogenic ( induced unintentionally by a physician or surgeon or by medical treatment or diagnostic procedures) causes of toxicity can be seen when benzodiazepines are combined with other drugs during procedural sedation, particularly with opiates such as fentanyl.
The most common symptom of a benzodiazepine overdose is falling into a deep sleep or “coma” while still being able to breathe well enough. Other symptoms may include:
- Bluish-colored lips and fingernails
- Blurred vision, double vision
- Breathing is slow, labored, or stopped
- Confusion
- Depression
- Dizziness
- Drowsiness, lack of alertness
- Excitability
- Hiccups
- Rapid side-to-side movement of the eyes
- Rash
- Stomach upset
- Tiredness
- Tremor
- Weakness, uncoordinated movement
Before any diagnostic tests are ordered in the patient presenting with altered mental status with suspected overdose or toxicity, any respiratory or abnormal vital signs should be addressed first. Mechanical ventilation may be required to address respiratory compromise and intravenous fluids administered to manage hemodynamic instability.
Before Calling Emergency
Have this information ready:
- Person’s age, weight, and condition
- Name of product (ingredients and strength, if known)
- The time it was swallowed
- Amount swallowed
- If the medicine was prescribed for the person
The mainstay benzodiazepine overdose treatment is supportive care, which may include endotracheal intubation to provide definitive airway management. Single-dose or multi-dose activated charcoal, hemodialysis, or whole bowel irrigation play no role in managing benzodiazepine overdose and toxicity.
While the mainstay treatment of acute benzodiazepine toxicity or overdose is supportive care, there is, however, an “antidote for benzodiazepines” that may be used in limited situations. Flumazenil is a nonspecific competitive antagonist at the benzodiazepine receptor that can reverse benzodiazepine-induced sedation. However, in most cases, the risks of a flumazenil reversal agent for benzodiazepines usually outweigh the benefits in acute toxicity, and thus flumazenil is not recommended for routine benzodiazepine reversal.
Seizures and cardiac dysrhythmias can occur after flumazenil benzodiazepine antidote administration, and many fatalities have been reported. Flumazenil can precipitate acute withdrawal syndromes in those with chronic benzodiazepine dependence, which can be life-threatening. If a patient with a chronic dependence on benzodiazepines is given flumazenil as a benzodiazepines antidote dose, it can lower their seizure threshold and potentially cause life-threatening seizures. The treatment of seizures, which typically involves benzodiazepines, would be rendered useless, as the flumazenil has blocked the benzodiazepine receptors.
Flumazenil can be safely administered to non-habituated users of benzodiazepines. This situation classically occurs in the pediatric population with accidental ingestion or after procedural sedation. Flumazenil antidote of benzodiazepine is recommended that the decision to use flumazenil be based on the balance of risk versus benefit in the assessment and treatment of a patient that is a non-habituated user of benzodiazepines, as most people with a benzodiazepine overdose will do well with supportive care and time alone.
Acute Propofol and Benzodiazepine Intoxication
Propofol is an intravenous anesthetic used for procedural sedation, during monitored anesthesia care, or as an induction agent for general anesthesia. It may be administered as a bolus or an infusion, or some combination of the two. Propofol and benzodiazepines such as midazolam and lorazepam are commonly used for ICU sedation. However, Propofol causes dose-dependent respiratory depression due to the inhibition of the hypercapnic ventilatory drive. This respiratory depression is potentiated by the concurrent use of other sedative agents (benzodiazepines, opioids, central-acting alpha two agonists, or other anesthetic medications).

How to Treat Benzo Addiction
For those with substance use disorder or who know an individual suffering from benzo abuse, please consider treatment. The identification of a range of different drugs within counterfeit benzodiazepine tablets has been widely reported. Because this is an evolving situation, the benzodiazepine you use may contain other dangerous synthetic opioids.
Clearing benzos from the body and overcoming the risks of benzos and withdrawal are the goal of benzo detox, which is the first step of treatment for addiction.
We Level Up has a comprehensive team prescribing medications that can alleviate your withdrawal pains while monitoring your health 24 hours during the detox. We prioritize your safety and comfort because this is a fragile and challenging time for you.
Once detox is complete, a new doorway in treatment opens up, which is referred to as a residential level of care. The residential care program slowly and effectively introduces the individual into an atmosphere of therapeutic growth, marked by master’s level therapists, clinicians, group counselors, psychiatrists, and a community of like-minded individuals with the same aim: to attain sobriety and live a great life.
Some of the many modalities applied and practiced within our residential treatment facility are:
- Alumni Support
- Stabilization
- Holistic Therapy
If a friend or loved one begins expressing any of these behaviors, he or she may need professional help:
- Taking another person’s pills for his or her own use
- “Doctor shopping,” or visiting multiple doctors to obtain multiple prescriptions
- Forging prescriptions
- Stealing or borrowing a friend or loved one’s prescription
- Purchasing benzodiazepines illegally, such as through a street dealer
- Taking more benzodiazepines and/or over a longer period than first intended
- Spending significant time getting, using, and recovering from benzodiazepines
- Experiencing cravings or withdrawal symptoms
- Needing more of the benzo to achieve the same effect
- Exhibiting impaired performance at home, work, or school
People experiencing severe symptoms of substance abuse, co-occurring mental health disorders, or previous complicated withdrawals and relapses may greatly benefit from various inpatient drug rehab center programs. Inpatient rehabilitation facilities provide individuals struggling with alcohol or drug abuse with a structured, stable, and secure environment void of all temptations and distractions to help clients focus solely on their recovery. This inpatient drug rehab center also provides 24/7 support and medical care to help mitigate any medical complications during their stay.
While each individual in treatment will have specific long- and short-term goals, all specialized substance abuse treatment programs have three similar generalized goals.
- Reducing substance abuse or achieving a substance-free life
- Maximizing multiple aspects of life functioning
- Preventing or reducing the frequency and severity of relapse
Are you seeking a national inpatient rehab destination? We Level Up treatment tailors the program to the individual and the individual to the program of recovery. We begin by assessing our client’s history of mental health, drugs, and alcohol-related past. The needs of each patient are specific and personalized because we aim to provide comprehensive support for mental health, addiction, and dual diagnosis treatment. The supportive environment is designed accordingly to give patients 24-hour care for sobriety. Most importantly, we hope to have our clients live comfortably within the facility during this crucial and fragile time.
We Level Up prioritizes removing temptations for relapse and applying an air of recovery into every component of the treatment timeline. We Level Up finds that when clients are living in a supportive community, especially during their early recovery process, they can truly focus on what matters most: their recovery. If you or a loved one is struggling with the risks of benzos, reach out to We Level Up, and we can help you explore treatment options.
Programs, services, and treatments vary. We Level Up rehab center offers inpatient substance abuse treatment. Offering co-occurring treatments. We treat the entirety of addiction and behavioral health disorders including their secondary corresponding illnesses to improve long-term recovery outcomes. Get a free health assessment and find out what treatment options are most suitable for you. Call to learn more.
Xanax Addiction
Xanax is the benzodiazepine brand name for alprazolam. Alprazolam has been widely prescribed to treat anxiety and panic disorder and falls within the class of drugs known as benzodiazepines or central nervous system depressants. Side effects from the use of alprazolam include impaired psychomotor performance, impaired memory, ataxia, anterograde amnesia, paradoxical excitement, hypomania, and birth defects.
Xanax can be addictive, especially if a person believes they would be unable to manage their stress without it. Even persons who take Xanax as prescribed may get addicted to it. Tolerance to Xanax develops quickly, necessitating more frequent and higher dosages. As the person uses Xanax over time, their body and brain can develop a dependency on the drug, meaning that when they reduce their use or stop using altogether, they can experience withdrawal symptoms.
The desire to avoid withdrawal symptoms may lead some people to keep using Xanax. It is important to note that dependency is not the same as addiction. However, many individuals who develop Xanax benzodiazepines addiction are most likely dependent on the substance of abuse.
Restoril Detox
Temazepam is a safe hypnotic for use by older adults over an 8-week treatment period. There are few adverse effects and behavioral tolerance to those effects develops over time. Temazepam may cause physical dependence (a condition in which unpleasant physical symptoms occur if a medication is suddenly stopped or taken in smaller doses), especially if you take it for several days to several weeks. it is crucial that you do not stop taking this medication or take fewer doses without talking to your doctor.
Temazepam is an addictive benzodiazepine that causes the user to quickly acquire a tolerance and harsh withdrawal symptoms when they stop using it. Due to the possibility of dependency, many doctors advise using it for no more than 10 days at a time. Individuals prescribed the medicine should also be properly watched while on it if they develop tolerance.
Before receiving Restoril addiction therapy, a person must detox from it. This involves either going through withdrawal cold turkey on their own, gradually weaning down their dosage until it exits their system, or going through a supervised detox where they receive medical treatment while going through withdrawal. It is not advised to detox cold turkey owing to the risks associated with dehydration. At We Level Up detox center, we detox patients on a medical safety basis.
What are Roofies?
Rohypnol, the trade name for the drug flunitrazepam, is a central nervous system depressant. It is also known by its slang name “roofies” or a “date rape drug.” The drug is legally manufactured and available outside the United States but is neither manufactured nor approved for sale within the United States. Since the 1990s individuals in the United States have used Rohypnol illegally, often as a means of mitigating the depression that results from using stimulants such as cocaine and methamphetamine.
Flunitrazepam is a benzodiazepine chemically similar to prescription sedatives such as Valium® and Xanax®. Teens and young adults tend to abuse this drug at bars, nightclubs, concerts, and parties. It has been used to commit sexual assaults due to its ability to sedate and incapacitate unsuspecting victims.
Rohypnol is a strong sedative that can be used to treat insomnia or anxiety. This benzodiazepine is extremely addictive and can cause dependency and withdrawal symptoms. Individuals who quickly discontinue Rohypnol may develop withdrawal symptoms, including seizures. You are not alone in your struggle with Rohypnol withdrawal. Contact one of our treatment professionals now to learn more about Rohypnol withdrawal symptoms and to discover a medical detox facility near you.
Klonopin Addiction Treatment
Is Klonopin a benzodiazepines? Yes. Klonopin has the generic name of Clonazepam. It is a benzodiazepine commonly used to treat different conditions, including anxiety disorders and epileptic seizures. However, due to its low price and easy availability, it has become a widely misused medication in medical and recreational contexts. Someone can develop Klonopin addiction even if they take medication as prescribed by a healthcare provider.
Klonopin is a highly addictive benzodiazepine similar to Xanax, Ativan, and Valium. The medication is FDA-approved for panic and seizure disorders and is recognized for its long-acting, relaxing properties. It can also help with muscular spasms, sleep problems, mobility problems, and vertigo. Sadly, many people misuse their prescriptions or obtain Klonopin illegally. This type of abuse can lead to addiction.
The first step in overcoming a Klonopin addiction is to get professional assistance. We Level Up can assist you in having a safe, medically supervised detox from any substances you are attempting to quit. If you have a physical dependency on Klonopin, you must proceed with extreme caution while discontinuing the medication. Klonopin withdrawal may be severe, catastrophic, and even lethal. It is necessary to seek the advice of a doctor. But, with the proper care, you may safely discontinue Klonopin and begin the recovery process.
Ativan Addiction
Is Ativan a benzodiazepine? Yes. Ativan is a class of psychoactive drugs designed to help with chemical imbalances in the brain. You might also hear it as a sedative-hypnotic or anxiolytic medication. Many have been addicted to this drug and require Ativan detox to function normally again and avoid benzodiazepine side effects that bring health risks. Ativan addiction should not be taken lightly because all forms of substance abuse can lead to serious impairment.
Although Ativan may provide the desired benefits for some, prolonged usage of four weeks or more raises the likelihood of becoming physically dependent on the medication. When someone gets dependent on Ativan, stopping or reducing the dose might induce withdrawal symptoms. Since it inhibits the central nervous system, it can have hazardous consequences. When taken with other depressants, Ativan can induce overdosing, and it can also cause seizures if stopped abruptly.
While dealing with benzos, medical detoxification is essential. The procedure will gradually wean you off Ativan and build a medical strategy to assist you in fighting for your life. Addiction treatment experts will choose the best way ahead. It will suit your unique requirements as well as the safety standard. Thankfully, treatment can be personalized to meet your most individualized requirements.
How Dangerous is Valium? Valium Withdrawals & Addiction
Valium is a Schedule IV controlled substance with the potential for abuse. Development of dependence and tolerance can occur in addiction-prone, long-term treatment or those patients taking high doses. Thus, these individuals should be under careful supervision; once an individual develops dependence, the risk of developing withdrawal symptoms increases.
No one can deny the critical function Valium plays in assisting patients suffering from anxiety disorders, sleeplessness, or other psychiatric illnesses to manage their sickness. There is nothing to worry about if you follow your doctor’s advice and take the medicine under close medical supervision. But, if you are having difficulty controlling your cravings and meet the criteria for valium abuse, it is important to seek treatment and stop this habit before it becomes a hazardous problem.
Because Valium withdrawal may be dangerous, our clinically supervised, skilled intake team will assess whether a Valium detox is a good first step for you. You’ll like knowing that we bring no judgment to whatever your issue is, but simply factual, up-to-date information to help you recover the life you want to reclaim at each level of our admissions process.
Top 10 What is a Benzodiazepine? FAQs
-
Is Ambien a benzodiazepines?
Ambien benzodiazepines is not true. Ambien does not belong to the benzodiazepine class. It belongs to the sedative/hypnotic medication family and is mostly used to treat insomnia.
-
Is Gabapentin a benzodiazepine?
Gabapentin is not categorized as a benzodiazepine. Several research indicates that gabapentin can be utilized to treat benzodiazepine misuse and withdrawal. However, frequent use of gabapentin can lead to physical dependence on the drug, just like the effects of benzos.
-
Is Lexapro a benzodiazepines?
No. Lexapro is a selective serotonin reuptake inhibitor (SSRI). Selective serotonin reuptake inhibitors are a class of drugs that are typically used as antidepressants in the treatment of the major depressive disorder, anxiety disorders, and other psychological conditions.
-
Is Zoloft a benzodiazepine?
No. Zoloft is an antidepressant and not a controlled substance. Zoloft is an SSRI or selective serotonin reuptake inhibitor. However, Sertraline (Zoloft) can cause false-positive results for benzodiazepine in drug tests.
-
Is Hydroxyzine a benzodiazepines?
No. Hydroxyzine is an antihistamine medication. But Hydroxyzine can also be used to help control anxiety and tension caused by nervous and emotional conditions.
-
Is Prozac a benzodiazepines?
No. Prozac is a selective serotonin reuptake inhibitor (SSRI) antidepressant. It is used for the treatment of the major depressive disorder, obsessive–compulsive disorder, bulimia nervosa, panic disorder, and premenstrual dysphoric disorder.
-
Is Trazodone a benzodiazepines?
No. Trazodone is in a class of medications called serotonin modulators. It works by increasing the amount of serotonin, a natural substance in the brain that helps maintain mental balance.
-
Is Buspirone a benzodiazepine?
No. Buspirone is in a class of medications called anxiolytics. It works by changing the amounts of certain natural substances in the brain.
-
Is Clonidine a benzodiazepine?
No. Clonidine is in a class of medications called centrally-acting alpha-agonist hypotensive agents. Clonidine is used to treat high blood pressure, ADHD, drug withdrawal, menopausal flushing, diarrhea, spasticity, and certain pain conditions.
-
What is a benzodiazepines? Are benzodiazepines depressants?
Benzos are a group of depressant drugs. These drugs include alprazolam (Xanax®), chlordiazepoxide (Librium®), clorazepate (Tranxene®), diazepam (Valium®), halazepam (Paxipam®), lorzepam (Ativan®), oxazepam (Serax®), prazepam (Centrax®), and quazepam (Doral®).
Experience Transformative Recovery at We Level Up Treatment Centers.
See our authentic success stories. Get inspired. Get the help you deserve.
Start a New Life
Begin with a free call to an addiction & behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up Treatment Center Network delivers recovery programs that vary by each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- World-class Amenities
- Licensed & Accredited
- Renowned w/ 100s 5-Star Reviews
We’ll Call You
Search We Level Up Benzodiazepines Detox, Mental Health Topics & Resources
Sources
[1] Management of Benzodiazepine Misuse and Dependence – National Center for Biotechnology Information Brett J, Murnion B. Management of benzodiazepine misuse and dependence. Aust Prescr. 2015 Oct;38(5):152-5. DOI: 10.18773/austprescr.2015.055. Epub 2015 Oct 1. PMID: 26648651; PMCID: PMC4657308.
[2] Benzodiazepines – Drug Enforcement Administration
[3] Benzo Addiction Addiction – CBT Therapy For Addiction – We Level Up FL Dual-Diagnosis Center
[4] Alprazolam – U.S. Department of Health and Human Services National Institutes of Health
[5] Alprazolam is relatively more toxic than other benzodiazepines in overdose – National Center for Biotechnology Information Isbister GK, O’Regan L, Sibbritt D, Whyte IM. Alprazolam is relatively more toxic than other benzodiazepines in overdose. Br J Clin Pharmacol. 2004 Jul;58(1):88-95. DOI: 10.1111/j.1365-2125.2004.02089.x. PMID: 15206998; PMCID: PMC1884537.
[6] Oxazepam – U.S. Department of Health and Human Services National Institutes of Health
[7] Temazepam – U.S. Department of Health and Human Services National Institutes of Health
[8] Rohypnol – Drug Enforcement Administration
[9] Nitrazepam – National Center for Biotechnology Information PubChem [Internet]. Bethesda (MD): National Library of Medicine (US), National Center for Biotechnology Information; 2004-. PubChem Compound Summary for CID 4506, Nitrazepam; [cited 2023 Feb. 24]. Available from: https://pubchem.ncbi.nlm.nih.gov/compound/Nitrazepam
[10] Clonazepam for neuropathic pain and fibromyalgia in adults – National Center for Biotechnology Information Corrigan R, Derry S, Wiffen PJ, Moore RA. Clonazepam for neuropathic pain and fibromyalgia in adults. Cochrane Database Syst Rev. 2012 May 16;2012(5): CD009486. DOI: 10.1002/14651858.CD009486.pub2. PMID: 22592742; PMCID: PMC6485609.
[11] Lorazepam – National Center for Biotechnology Information Ghiasi N, Bhansali RK, Marwaha R. Lorazepam. [Updated 2022 Nov 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532890/
[12] Diazepam – National Center for Biotechnology Information PubChem [Internet]. Bethesda (MD): National Library of Medicine (US), National Center for Biotechnology Information; 2004-. PubChem Compound Summary for CID 3016, Diazepam; [cited 2023 Feb. 24].





