Opiate Detox Timeline, Withdrawal Symptoms, & Top Treatment Options
Opiate withdrawal is a life-threatening condition resulting from drug dependence. Opiates refer specifically to drugs derived directly from the opium poppy, such as morphine and codeine. However, the distinction between opioids and opiates is becoming less relevant as synthetic opioids become more common and natural opiates are synthesized into semi-synthetic opioids. Read more about opiate detox and the benefits of getting professional medical help.
By We Level Up | Editor Yamilla Francese | Clinically Reviewed By Lauren Barry, LMFT, MCAP, QS, Director of Quality Assurance | Editorial Policy | Research Policy | Last Updated: May 5, 2023
Opiate Detox Overview
Individuals struggling with opioid addiction who meet the diagnostic criteria for substance use disorder need medical support when detoxing from opiates. Opioids and opiates are a powerful class of naturally occurring and synthetic drugs. These drugs are widely used for pain management capabilities and are commonplace in managing moderate and severe (and often chronic) pain. However, due to how opiates affect the body, these drugs can cause sedative and euphoria-inducing effects, making them a target of abuse.
As a result, the illegal types of opioids (heroin, fentanyl) and legal opiates, and opioid varieties (codeine, oxycodone, hydrocodone) have become popular recreational drugs. Furthermore, the distinction between “opioids” and “opiates” is becoming less relevant as synthetic opioids become more common and natural opiates are synthesized into semi-synthetic opioids.
Regular use of opiates leads to an incapacitating form of addiction in users. Opioid dependency influences the drug user and inflicts a significant societal problem by increasing healthcare costs, unemployment rates, absenteeism, and premature death. This article will tackle the timeline, symptoms, and different levels of care for clients to enter after and before completing their opiate detox programs. When someone is experiencing withdrawal symptoms from opiates, it’s best to get them medical help as early as possible.
Opiate Withdrawal Timeline
How long does it take to withdraw from opiates? The timeline of opiate withdrawal is determined by several factors, such as the specific drug used, the dosage, and the duration of use.
Below are the general stages of opiate withdrawal after discontinuing.
| First 24 hours. | Early opiate withdrawal symptoms usually start within 12 hours of the last dose, including muscle aches, agitation, anxiety, and insomnia. |
| Days 2-4. | Symptoms typically peak around this time, including nausea, vomiting, diarrhea, abdominal cramping, sweating, and chills. |
| Days 5-7. | Symptoms begin to subside, but physical and psychological symptoms can still occur, including depression, mood swings, and fatigue. |
| Days 8-14. | Opiate withdrawal symptoms continue to improve, but some may experience lingering symptoms, such as insomnia and mood swings. |
How long do opiate withdrawals last? The period and extent of opiate withdrawal symptoms also depend on whether the opioid is long-acting or short-acting.
Heroin is relatively short-acting compared to other opiates. Therefore, heroin withdrawal symptoms appear just hours after the last dose and may last for a shorter period. On the other hand, longer-acting opioid painkillers may not provoke withdrawal symptoms till some days after the final amount, and some symptoms may last for weeks.
Opiate Withdrawal Symptoms
What are the symptoms of opiate withdrawal? Opiate withdrawal can be a significant problem for people physically dependent on these drugs.
When someone stops using opiates after prolonged use, their body may react with a range of withdrawal symptoms, which can be severe and uncomfortable.
Early Opiate Withdrawal Symptoms (usually within 12 hours of the last dose)
- Muscle Aches.
- Agitation.
- Anxiety.
- Insomnia.
- Runny nose.
- Sweating.
Acute Opiate Withdrawal Symptoms (usually peak within 2-4 days)
- Nausea.
- Vomiting
- Diarrhea.
- Abdominal cramping.
- Sweating.
- Chills.
- Fever.
- Rapid heartbeat.
- High blood pressure.
- Dilated pupils.
- Goosebumps.
Late Opiate Withdrawal Symptoms (can last up to a week or more)
- Depression.
- Anxiety.
- Irritability.
- Mood swings.
- Insomnia.
- Fatigue.
- Loss of appetite.
What Does Opiate Withdrawal Feel Like?
Opiate withdrawal yawning is common for people who are detoxing opiates. During opiate use, opioids can suppress the regular respiratory drive in the brain, which can result in reduced breathing rate and oxygen levels in the body. When a person stops using opioids, their body tries to restore the average breathing rate, which can increase respiratory rate and volume, including yawning.
Opiate withdrawal symptoms can be both physical and psychological. Physical symptoms may include nausea, vomiting, diarrhea, abdominal cramps, muscle aches and pains, runny nose, chills, sweating, and goosebumps.
These symptoms are often accompanied by intense cravings for the drug, which can be difficult to resist and may lead to relapse.

Skip To:
Learn More:
- Opiate Withdrawal Symptoms, Can You Die From Opiate Withdrawal?
- How Long Do Opiates Stay in Your System, Body, Blood, and Urine?
- Opiate Addiction
- Opiate Withdrawal Restlessness
- Opioid Overdose Symptoms
- Opioid Withdrawal Symptoms
- Opioid Crisis
- Opioid Addiction Treatment
- Medical Detox Treatment
- Opioid Withdrawal Timeline
Opiate Withdrawal Protocol Fact Sheet
Medical Detox From Opiates
Opiate withdrawal protocols are determined by the individual’s needs and the healthcare provider’s treatment approach. However, several general steps are typically included in an opiate withdrawal protocol, such as the following:
- Assessment: The first step in an opiate withdrawal protocol is to assess the individual’s physical and psychological health, including any underlying medical conditions, history of substance use, and mental health concerns.
- Stabilization: Once the assessment is complete, the healthcare provider will work to stabilize the individual, including managing any acute medical or psychiatric issues and ensuring the individual is safe and comfortable.
- Medication-Assisted Treatment (MAT): MAT with opiate withdrawal medications, such as buprenorphine, methadone, or naltrexone, are often used. These medications reduce withdrawal symptoms and cravings and can be used in inpatient and outpatient settings.
- Behavioral Therapy and Counseling: Medication, behavioral therapy, and counseling are often included in an opiate withdrawal protocol to help individuals address the underlying causes of their substance use disorder and develop coping skills to manage cravings and triggers.
- Follow-Up Care: After completing opiate withdrawal treatment, follow-up care is crucial for maintaining long-term recovery. This can include ongoing medication management, counseling, and support group meetings.
Opiate Addiction
No matter what the narcotic is, ongoing use can lead to developing a physical dependency. When this occurs, the body has become so used to a sense that it often requires it to function. Psychological cravings usually follow shortly after that, resulting in what is known as full-blown addiction.
In the case of opiates, the risk of developing an addiction is significantly higher due to parts of the brain that are stimulated by opioid use. Opioids activate our mu-receptors, which influence the sensations of both pain and pleasure.
Feelings of happiness are closely related to reward pathways in the brain, and once triggered, it creates a strong association that can quickly lead to the development of compulsive behaviors. Opiates can do this on a powerful level that can be up to 10x more intense than the feelings of pleasure our bodies usually produce. Opioid highs have been described as a “wave of euphoria” and can be so powerful as to rewire the brain, leaving it wanting more after a single use.
In many cases, the abuse of opioid painkillers is not detected early enough to prevent a physical addiction. Sadly, many addicts taste their drug of choice (DOC) for the first time after they’ve been prescribed opioids by a doctor. Typically, younger people have become addicted to opiates due to injuries sustained by playing competitive sports, automobile accidents, etc. This particular addiction leads to hazardous behaviors. Social pressure and other illicit drugs can also lead to the abuse of illegal opioids.
Some signs of severe opiate addiction or the use of illicitly made opioids include the following:
- Withdrawal from everyday activities.
- Possession of drug paraphernalia (mental spoon, glass pipe, syringe, lighter, candle & matches).
- Doctor shopping. (going to multiple doctors to receive prescriptions)
- Going to numerous pharmacies around town to fill prescriptions.
How Long Do Opiates Stay In Your System?
Most opiates can be detected in urine for 2-4 days after use. However, some opiates, such as methadone, can stay in the system for 2-3 weeks. Hair and blood tests can detect opiates for a more extended period, up to 90 days in some cases. The detection window is determined by the type of drug test used and the test’s sensitivity. Moreover, chronic or heavy opiate use can increase the time that opiates stay in the system.
Narcotics Drug Fact Sheet
Download below DEA’s “Narcotics Drug Fact Sheet” for further information about opiates. This file has been made publicly available for downloading to help substance use disorder awareness.

Get Your Life Back
Find Hope & Recovery. Get Safe Comfortable Detox, Addiction Rehab & Dual Diagnosis High-Quality Care.
Hotline(844) 597-1011Opiate Addiction Recovery Statistics
According to the CDC, opioid-related fatalities have skyrocketed in the recent decade, accounting for nearly 70% of drug-related overdoses in 2018. These numbers include illicit and prescription opioid drugs. But it has primarily been the latter that has driven the ongoing epidemic crisis in the United States. Unfortunately, the hundreds of thousands of individuals who are already physically dependent on these substances must face the reality of opioid and opiate detox, withdrawal, and rehab if they can get their recovery on track and build a better life. Fortunately, we do recover.
91%
Analyses have reported alarming relapse rates with opiate abuse compared to other drugs. One study reported a relapse rate of up to 91 percent in opiate addicts, implying that the risk for relapse could be higher for opiate addiction than other drug addictions.
Source: NCBI
9.3 Million
In 2020, 3.3 percent (about 9.3 million individuals) reported misusing prescription pain drugs in the past 12 months.
Source: NIDA
50%
Individuals with opioid use disorder are less likely to die when they are in long-term treatment with buprenorphine or methadone than when they are untreated. Therapy using agonist medication is linked with an estimated death reduction of approximately 50 percent among individuals with opioid addiction.
Source: NCBI
Top 10 Opiate Withdrawal Remedies FAQs
-
Does alcohol help opiate withdrawal?
No. Alcohol is not recommended as a means to manage opiate withdrawal symptoms. Although alcohol drinking can have a sedating effect, it can also be addictive and cause harm to the body. Combining alcohol with opiates can be dangerous, as both substances can cause respiratory depression and increase the risk of overdose. Does alcohol help with opiate withdrawal? Instead of alcohol, medication-assisted treatment (MAT) is recommended to manage opiate withdrawal symptoms.
-
Does Suboxone help with opiate withdrawal?
Suboxone (Buprenorphine and Naloxone) is an effective medicine to help with opiate withdrawal symptoms. Suboxone is a medication-assisted treatment (MAT) that combines Naloxone, an opioid antagonist, and buprenorphine, a partial opioid agonist.
-
Can you take Ketamine for opiate withdrawal?
Ketamine is not typically used as a treatment for opiate withdrawal, and current medical guidelines do not support its use. Ketamine is a dissociative anesthetic used primarily for anesthesia and pain relief. It is not an opioid drug and does not produce the same effects on the brain and body as opioids. Although some research has suggested that Ketamine may have potential as a treatment for depression and drug addiction, more research is required to determine its safety and efficacy for these conditions.
-
Is it effective to take Lyrica for opiate withdrawal?
Lyrica (pregabalin) is not approved by the U.S. Food and Drug Administration (FDA) to treat opiate withdrawal. However, some healthcare providers may prescribe Lyrica off-label to manage opiate withdrawal symptoms. Lyrica is an anticonvulsant medication for treating various conditions, including seizures, anxiety, and neuropathic pain.
-
What is the use of Hydroxyzine for opiate withdrawal?
Hydroxyzine is an antihistamine medication sometimes used off-label to manage opiate withdrawal symptoms. It works by blocking histamine receptors in the brain, which can help reduce anxiety and improve sleep. Hydroxyzine is not approved by the U.S. Food and Drug Administration (FDA) for treating opiate withdrawal, but it may be prescribed off-label as part of a comprehensive treatment plan.
-
How to obtain Tramadol for opiate withdrawal?
Tramadol is a synthetic analgesic that functions centrally, having opioid-like effects, yet with low potential for abuse. Several clinical analyses executed in the past ten years have recognized the impact of Tramadol in opioid withdrawal cases. To obtain Tramadol for opiate withdrawal, you must work with a healthcare provider who can assess your specific needs and develop a treatment plan. Tramadol is a prescription medication, so that you will need a prescription from a licensed healthcare provider, such as a doctor or nurse practitioner. Your healthcare provider will likely assess your medical history and perform a physical examination to determine the appropriate dose of Tramadol and the length of treatment needed. They may also recommend additional medications or therapies to manage withdrawal symptoms and support long-term recovery.
-
Is Baclofen for opiate withdrawal effective?
Baclofen is a muscle relaxant medication used off-label to manage opiate withdrawal symptoms. It works by activating a specific type of receptor in the brain that regulates the release of dopamine, a neurotransmitter often disrupted during opiate withdrawal. Baclofen opiate withdrawal medicine should only be used under the guidance of a healthcare provider experienced in treating opiate addiction and withdrawal. They can evaluate your needs and develop a personalized treatment plan considering your medical history, current symptoms, and treatment goals.
-
Are detox drinks for opiates sufficient?
Detox drinks for opiates are marketed as products that can help eliminate traces of opioids from the body, allowing individuals to pass drug tests or reduce withdrawal symptoms. However, there is little scientific proof to support the effectiveness of these products. Some detox drinks may even be harmful, as they contain ingredients that can cause adverse reactions or interfere with other medications. It’s crucial to be cautious when using any detox product and to seek guidance from a healthcare provider before starting any new opiate withdrawal meds or supplements.
-
What is an opiate rapid detox?
Opiate rapid detox is a treatment for opiate addiction that involves using anesthesia and other medications to rapidly and forcibly induce withdrawal symptoms while the patient is sedated. The goal of rapid detox for opiates is to accelerate the withdrawal process, allowing the patient to complete detoxification in a matter of hours instead of days or weeks. Are you searching for a “rapid opiate detox near me?” While opiate rapid detox can appeal to individuals who want to complete detox quickly and avoid the discomfort of withdrawal, it is not without risks. The procedure can be expensive and not covered by most insurance plans. Moreover, there is a risk of severe medical complications, including heart attack, stroke, and death.
-
Can you take Loperamide for opiate withdrawal?
Loperamide is an over-the-counter medication that is commonly used to treat diarrhea. Imodium for opiate withdrawal works by slowing bowel movements and reducing the frequency and severity of bowel movements. While Loperamide is not an opiate itself, it works on the same receptors in the gut as opiates do, which means it may help alleviate some of the gastrointestinal symptoms that often accompany opiate withdrawal, such as diarrhea and abdominal cramping. However, Loperamide should not be used as part of the primary meds for opiate withdrawal. It is ineffective at managing other withdrawal symptoms, such as cravings, anxiety, and insomnia, and it does not address the underlying addiction.
Get Help. Get Better. Get Your Life Back.
Searching for Accredited Drug and Alcohol Rehab Centers Near You?
Even if you have failed previously and relapsed, or are in the middle of a difficult crisis, we stand ready to support you. Our trusted behavioral health specialists will not give up on you. When you feel ready or just want someone to speak to about therapy alternatives to change your life call us. Even if we cannot assist you, we will lead you to wherever you can get support. There is no obligation. Call our hotline today.
(844) 597-1011Addiction To Prescription Opiates
The opioid epidemic exploded in the 90s and has gained more momentum in recent years. Thanks to modern technology, more accurate information is publicly available. Subsequently, people are somewhat more attentive to what doctors prescribe. Unfortunately, it does not take long to develop a dependence on them. Therefore, if you notice any of the following regarding your or a loved one’s use of a prescription opioid, you should contact an addiction specialist for help.
Opiate addiction, also known as opioid use disorder, is a chronic condition characterized by the compulsive use of opioids despite the negative consequences that it may have on a person’s health, relationships, and other areas of their life. Opiates are a class of medications that include painkillers like oxycodone, hydrocodone, and morphine, as well as illicit drugs like heroin. When taken in high dosing or for a prolonged period, opiates can cause physical dependence, which implies that the body adapts to the medication’s presence or drug and needs it to function normally.
Signs of Opioid Addiction
It’s crucial to seek professional addiction help if you or somebody you care about has an opiate addiction, as it is a severe and potentially life-threatening condition.
- Taking frequent doses or larger doses to feel the same effect.
- Inability to stop or control the use.
- Uncontrollable cravings.
- Failure to perform at work, school, or fulfill personal obligations.
- Continued use despite consequences that negatively impact your life.
- Isolating; Withdrawn from social situations.
- Inability to stop despite mental or physical health concerns.
- Opiate withdrawal symptoms.
Opiate Withdrawal Treatment
When the substance is suddenly absent, the body responds with unpleasant withdrawal symptoms ranging from flu-like to potentially fatal. For this reason, it is recommended to taper off opioid use slowly rather than quitting cold turkey and, ideally, with the supervision of a medical professional. Fortunately, several opioid antagonists can help beat opioid addiction at difficult stages. These medications can help mitigate the signs of opiate withdrawal or intervene in an opium overdose.
Naloxone is the generic name of a drug that can reverse the opioid overdose effects. It acts by attaching itself to the same receptors occupied by the harmful opioids and taking their place. By disrupting the connection between the deadly opioid and the receptor, Naloxone can immediately reverse the adverse effects of an overdose. This can be life-saving, namely by restoring the ability to breathe.
It is obtainable as an injectable liquid and as a nasal spray. The most common brand names include Narcan and Evizo. This medication is only effective if administered when an overdose occurs and cannot be used pre-emptively to prevent an opioid overdose.
This opiate detox medicine functions similarly to methadone, another opioid antagonist commonly used to treat opioid dependence. However, methadone has recently fallen out of favor as a treatment for opioid addiction due to its potential for habit-forming. As such, it has largely been replaced by buprenorphine in addiction treatment settings.
Buprenorphine shot for opiate withdrawal can activate opioid receptors and relieve cravings without eliciting any surge of euphoria. Thus, being an opioid can fulfill the receptors’ physical need to be stimulated but does so without generating feelings of joy (the leading cause of addiction-forming behavior).
What makes it even more helpful is the limits on the effect this partial opioid can exert on these receptors. This ensures that It can achieve no high, effectively eliminating the likelihood of being abused, and limits the effects of other opioids.
Suboxone is a brand-name drug composed of Naloxone and Buprenorphine used to treat opioid dependence, not just manage the common symptoms of withdrawal from opiates. The buprenorphine component can lessen persisting opioid cravings, the primary side effect of opioid detox or withdrawal.
The presence of Naloxone allows Suboxone to take treatment a step further. Instead of reversing the symptoms of an overdose, Naloxone acts as a deterrent to further opioid abuse. It does so by causing unpleasant withdrawal symptoms should Suboxone be used via injection (a typical administration method for drug abusers) instead of being taken orally as directed. This prevents Suboxone users from trading one addiction for another.
Benzos for Opiate Withdrawal
Does Xanax help with opiate withdrawal? The use of benzodiazepines, or “benzos,” such as Xanax, for opiate withdrawal is generally not recommended due to the potential risks and complications associated with their use.
Benzodiazepines are a class of medications that are commonly used to treat anxiety, insomnia, and other conditions. While Xanax for opiate withdrawal can effectively manage some opiate withdrawal symptoms, it can also be highly addictive. It can cause various side effects, including dizziness, confusion, and respiratory depression.
When combined with opioids, benzodiazepines can increase the risk of overdose and other serious complications. Moreover, they can also increase the risk of addiction and withdrawal symptoms when used for prolonged periods.
It’s vital to consult with a healthcare professional before taking any medication for opiate withdrawal, as they can help determine the most appropriate treatment approach based on the unique requirements of each and medical history.
Cannabidiol for Opiate Withdrawal
Cannabidiol, a compound known as CBD, is a non-psychoactive chemical found in the cannabis plant. It has been researched for its possible therapeutic effects. While there is limited research on the use of CBD for opiate withdrawal specifically, some studies suggest that it may help manage some of the symptoms associated with opiate withdrawal. However, no substantial evidence supports CBD as a primary treatment for opiate withdrawal. More CBD opiate withdrawal research is needed to understand its potential benefits and risks fully.
Does Gabapentin Help Opiate Withdrawal?
Yes, Gabapentin helps manage some of the symptoms of opiate withdrawal. Gabapentin is an anticonvulsant medication commonly used to treat seizures, nerve pain, and other conditions. It works by reducing the activity of certain neurotransmitters in the brain and nervous system, which can help to relieve symptoms such as anxiety, insomnia from opiate withdrawal, and restlessness. In some studies, Gabapentin effectively reduces the severity of withdrawal symptoms in people undergoing opiate detoxification. It may be particularly helpful in managing symptoms such as anxiety, pain, and opiate withdrawal insomnia.
However, Gabapentin for opiate withdrawal can have side effects and may not be suitable for everyone as a medicine opiate withdrawal management. Common side effects of Gabapentin opiate withdrawal medicine include dizziness, drowsiness, and difficulty concentrating. Opiate withdrawal Gabapentin medication can also be habit-forming and may cause withdrawal symptoms if stopped abruptly.
Clonidine for Opiate Withdrawal
Many are considering Clonidine opiate withdrawal dosing as a treatment. But how does Clonidine help with opiate withdrawal? Clonidine is a medication that helps manage some of the symptoms of opiate withdrawal. Clonidine dosage for opiate withdrawal can help relieve symptoms such as anxiety, agitation, insomnia, elevated heart rate, and blood pressure.
Clonidine dose for opiate withdrawal does not function as a pain reliever; it does not directly address the physical symptoms of opiate withdrawal, such as muscle aches and cramps. However, reducing the severity of withdrawal symptoms can help people undergoing opiate detoxification tolerate the process better and reduce the risk of relapse.
Vitamin C for Opiate Withdrawal
Little scientific proof supports the use of vitamin C specifically for opiate withdrawal. However, vitamin C is essential in many bodily functions, including collagen synthesis and immune function. Some research has suggested that vitamin C may benefit from managing drug withdrawal symptoms. However, vitamin C should not be used as a substitute for evidence-based treatment approaches, such as medication-assisted treatment, counseling, and behavioral therapies.
Does Kratom Help With Opiate Withdrawal?
Kratom is an herbal supplement used for centuries in Southeast Asia as a natural medicine for fatigue, anxiety, and pain. Some people have suggested that the kratom dose for opiate withdrawal may also help manage withdrawal symptoms.
While there is limited kratom opiate withdrawal research, some studies have suggested that it may reduce the severity of withdrawal symptoms and improve mood in people with substance use disorders. However, there is not yet enough high-quality evidence to support using the best kratom for opiate withdrawal as a primary treatment for opiate withdrawal.
Trazodone for Opiate Withdrawal
Trazodone is a medication that is commonly used to treat depression and anxiety. While it is not explicitly indicated for treating opiate withdrawal, it has been used off-label to help manage specific withdrawal symptoms. Trazodone is a SARI (serotonin antagonist and reuptake inhibitor) that increases serotonin levels in the brain. This can help to alleviate symptoms such as anxiety, depression, and insomnia that can occur during opiate withdrawal. However, trazodone may not suit everyone and can have side effects. Trazodone can interact with other medications and should be used cautiously in people with certain medical conditions, such as heart disease and liver or kidney problems.
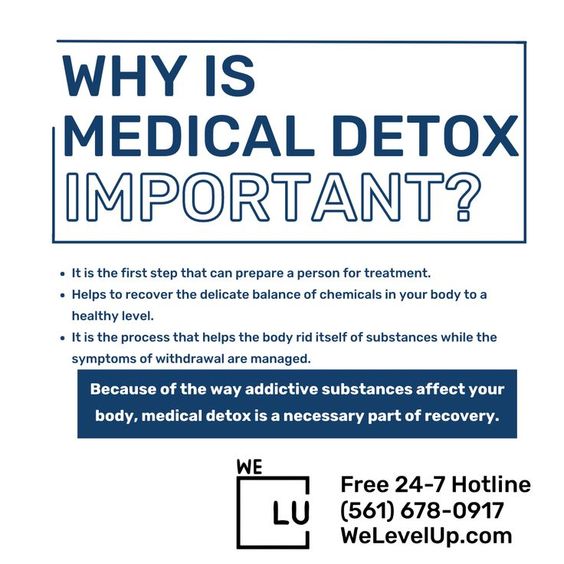
Opiate Detox at Home
Home remedies for opiate withdrawal can be difficult and sometimes unproductive. Unaided withdrawal may not be life-threatening, but there is a significant possibility that it will lead to relapse. When opioid substances such as oxycodone and heroin begin to leave the human blood system, they develop severe cravings for the substance. Intense cravings and unpleasant flu-like symptoms can make it easy for someone going through withdrawal at home to give up and relapse before their recovery gets in its way.
Without the medical and opiate withdrawal specialists’ support that a detox center offers, it is tempting to abandon withdrawal and start using again. The drugs to help with opiate withdrawal and therapy are accessible at a medical detox center to help reduce the discomfort and the risk of relapse compared to detoxing at home.
Opiate Detox Centers Near Me
How to help opiate withdrawal? Treatment programs for opioid addiction usually start with the “opiates detox,” followed by inpatient treatment or some specified treatment procedure (partial hospitalization or concentrated treatment programs). Only a finely managed treatment facility provides a controlled and comfortable setting to detox opiates. Drug detox can occur while providing support and opiate withdrawal supplements or medications to help decrease the possibility of complications and difficulties associated with opiate withdrawal.
If you’re looking for an “opiate detox Florida,” “opiate detox Orange County,” or “Los Angeles opiate detox,” contact We Level Up nationwide helpline for resources and options near you. Opiate detox at a medically supervised facility can minimize the severity of the symptoms and make the withdrawal process significantly more manageable and more comfortable to endure. Our facilities also offer multiple levels of treatment for an easy transition following the completion of an opiate detox program.
Amenities at We Level Up include semi-private rooms, luxurious bathrooms, spacious common areas for socializing, a communal dining area always stocked with nutritious snacks, and much more!
Opiate Detox Process
The opiate detox process is not the same as detoxing from other addictive substances, such as alcohol or cocaine. The withdrawal symptoms are different, and medications are often used to help minimize the physical withdrawal symptoms and prevent the intense cravings accompanying opioid detox. Detox from heroin, fentanyl, and prescription opioids is a closely managed process, and often the same or similar medications are continued to be used following detox.
Medications such as Subutex and Suboxone have been officially approved by the Food and Drug Administration (FDA) to treat opioid dependence. These new medications have opened up various opioid detox treatment methods. The opioid detox process will differ for individuals detoxing via medically assisted treatment versus abstinence.
Opiate Detox Medications
Medical opioid detox helps smooth withdrawal, reduce side effects, prevent serious complications, and lessen opioid cravings. Some of the most common opiate withdrawal shots and medications are the following:
- Buprenorphine: Prescribed to reduce the period it takes for opiate detoxification and assists an individual in upholding prolonged abstinence from opioids. The commonly used brand name of this substance is Subutex. Suboxone is a drug that includes both buprenorphine and Naloxone.
- Methadone: Relieves and reduces the unpleasant impact of withdrawal symptoms.
- Naltrexone: Blocks the effects of opioids and may be used to induce withdrawal. It does not let the opioid intake affect the individual. Therefore, It may also use to avert future dependence and misuse.
- Clonidine: Can help diminish the flu-like symptoms that come with opioid withdrawal, along with other withdrawal symptoms such as the anxiety and agitation most people experience.
These prescriptions and supplements for opiate withdrawal offer a decent start toward recovery and help maintain long-term sobriety. However, detox must be followed with counseling, education, and awareness. Family, individual therapy, and support groups can aid an individual in stopping using drugs and continuing sobriety.
What to Expect from an Opioid Detox Center?
The We Level Up opioid addiction treatment center is here to help individuals complete the opioid detox process and address psychological, physical, and spiritual issues connected to drug abuse.
Qualified specialists, doctors, nurses, therapists, and addiction case managers will be with you throughout the recovery process to ensure you have the support you need.
Recovering from opiate addiction is never easy, but We Level Up’s opiate detox facility can make the process much more comfortable. The team at our medical detox program is dedicated to helping people break through this difficult first stage of recovery while preparing them for the next steps in the addiction therapy process.
The first steps at a detox center typically include a detailed assessment. When you first enter our facility, our team will ask you about your drug use history, including how long you’ve been using opiates, how frequently, and what your typical dose was. This information helps our team develop a personalized treatment plan to manage your acute withdrawal symptoms.
In addition, we will screen for any preexisting medical or mental health conditions that could impact your course of treatment. If you have preexisting conditions, there’s no need to be alarmed; our opiate detox programs are equipped to help manage a wide range of health concerns, and you can still get the help you need to overcome opiate addiction.
During Treatment
During your stay at detox, you will be under 24/7 medical supervision to ensure that your opiate withdrawal symptoms are under control. Acute withdrawal symptoms can last for up to two weeks, and the targeted medications offered at our opiate detox center can help them stay manageable.
Attending inpatient detoxification is an all-inclusive experience. Our team takes care of all of life’s necessities so you can focus on feeling better and working toward overcoming your opiate addiction. That includes meals, healthcare services, medication schedules, and much more.
The main focus of an opiate detox center is to help people overcome the physical symptoms of opiate withdrawal. While you might also receive treatments that can help you manage psychological symptoms, much of your time in detox is spent relaxing and engaging in practices that can ease the physical discomfort associated with withdrawal.
We encourage detox clients to bring items to help them pass the time and distract them from their symptoms. You might consider activities like these:
- Reading a book.
- Making art.
- Writing in a journal.
- Creating small crafts.
- Knitting.
Keeping focused on a hobby or interest can help individuals get through the first few days of detox while they receive medical treatment.
Leaving Detox
Before you leave detox, our team makes a complete and detailed transition of the care plan for the next stage in your treatment. While medical detox is a vital first step, it must be followed by intensive addiction treatment to support long-term recovery.
At We Level Up, we have streamlined this process to be as simple as possible. Our treatment network spans the entire continuum of care, and our residential treatment centers, partial hospitalization programs, and medical detox facilities work together for client transitions. When seeking care at We Level Up, you won’t have to wait for a bed or be unsure where to go after detox.
What Happens After Opiate Detox?
We Level Up offers several different levels of care for clients to enter after completing their opiate detox programs. Each of these programs provides evidence-based treatment methods with decades of research proving their effectiveness in helping people overcome opiate addiction.
Residential Treatment
Most clients will enter residential treatment after completing an opiate detox program. Residential treatment is the most intensive drug and alcohol therapy model available, with clients living on-site at a treatment facility with other people working toward recovery.

During the day, clients attend several different therapies and groups designed to help them overcome opiate addiction, including these evidence-based treatments:
- Individual therapy.
- Group therapy.
- Relapse prevention programs.
- Motivational interviewing.
- Medication-assisted treatment.
- Family therapy.
Together, these techniques help people manage the lingering symptoms of opiate addiction, learn healthy coping mechanisms to deal with future stressors and develop relapse prevention skills that can last a lifetime.
Dual-Diagnosis Treatment
Dual-diagnosis treatment is designed to help people dealing with addiction and mental illness. Mental health conditions such as depression, panic attacks, anxiety, and post-traumatic stress disorder are pervasive among people with opiate addictions. They can be a serious roadblock on the path to recovery if left untreated.
These mental health disorders can exist before substance use begins or may develop due to months or years of active addiction. Whatever the case, a dual-diagnosis treatment facility can help. In a dual-diagnosis program, effective mental health treatment is integrated with evidence-based treatment for substance use disorders. This could include treatments such as:
- Psychiatric evaluations.
- Medication management.
- Cognitive-behavioral therapy.
- Eye movement desensitization and reprocessing.
- Dialectical behavior therapy.
A dual-diagnosis program offers these therapies alongside all the treatments for substance use disorders. Untreated mental health challenges can drastically increase the risk of relapse after leaving an intensive program. Dual-diagnosis treatment offers an additional defense against relapse by treating mental illness and addiction symptoms simultaneously.
Many people can achieve remission from their mental health concerns with targeted treatment. Those who don’t achieve total remission may still experience a significant reduction in symptoms, which might be just what it takes to achieve lasting sobriety.
Opiate Detox Treatment
Opioid addiction is a deadly, life-threatening disease that can have irreversible effects on one’s health and relationships. Without help, this addiction will more than likely turn deadly. Immediate professional help and opiate detox are the only way to avoid overdose risk and harm to yourself or a loved one. Contact our treatment support at We Level Up to find the best treatment option.
Your call is private and confidential, and there is never any obligation.
First-class Facilities & Amenities
World-class High-Quality Addiction & Mental Health Rehabilitation Treatment
Rehab Centers TourRenowned Addiction Centers. Serene Private Facilities. Inpatient rehab programs vary.
Addiction Helpline(844) 597-1011Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Success Stories Across Our Network
- Low Patient to Therapist Ratio
- Onsite Medical Detox Center
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Personal Development Events
Types of Opioids / Opiates
There is a wide array of opioids in the U.S. Some are prescription drugs used in a medical setting to manage severe pain, whereas others are illicitly made and abused. Learn more about some of the most common and dangerous opiate and opioid addictions:
Heroin Detox
Heroin addiction can have many adverse effects on a person’s life. It can lead to financial, legal, relationship, and physical and mental health problems. Overdose is a significant risk for people with heroin addiction, as the drug can depress the respiratory system and lead to coma or death.
Treatment for heroin addiction typically involves a combination of medications and behavioral therapies. Certain drugs can support and manage withdrawal symptoms, reduce cravings, and avoid relapse. Behavioral treatments such as cognitive-behavioral therapy, motivational interviewing, and contingency management can help people with heroin addiction develop coping skills, improve problem-solving abilities, and maintain abstinence from drug use.
What is Hydrocodone?
Hydrocodone is a semi-synthetic opioid prescription drug for treating moderate to severe pain. It is obtainable in different forms, including tablets, capsules, and syrups. Hydrocodone is classified as a Schedule 2 controlled substance in the U.S., which means it has a high potential for drug addiction and dependency.
What is Oxycodone?
Oxycodone binds to the brain’s opioid receptors and spinal cord, which aids in blocking pain signals and reducing pain perception. It is often used with other pain relievers, such as ibuprofen and acetaminophen, to enhance its pain-relieving effects. Because of its potential for drug addiction and dependence, oxycodone should only be used under the close supervision of a healthcare provider, and patients should be closely monitored for indications of misusing drugs, dependence, or addiction.
Percocet Detox
Percocet is a prescription pain medication that combines oxycodone and acetaminophen. It is a powerful opioid that can lead to physical dependence and addiction with prolonged use. A medical detox program is often recommended for people dependent on Percocet. This involves a supervised withdrawal process in a safe and controlled environment, typically in an inpatient or addiction treatment center. During detox, patients may receive medications to manage their withdrawal symptoms and help them stay comfortable.
Morphine Addiction
Morphine is a powerful opioid medication used to treat severe pain. It works by binding to the opioid receptors in the brain, blocking pain signals, and producing euphoria and relaxation. Morphine has a high potential for addiction and dependence, particularly long-term use. Regular use of morphine can lead to physical dependence, meaning that the body has adapted to the drug’s presence, and withdrawal symptoms will occur if it is discontinued.
What is Codeine?
Codeine is an opioid medication commonly used to treat pain and cough. With prolonged use, codeine can cause physical dependence and addiction, and withdrawal symptoms can occur when the drug is discontinued. Withdrawal from codeine can be uncomfortable, but it is usually not life-threatening. However, it is crucial to seek professional help when detoxing from codeine, as attempting to detox on your own can be dangerous and may lead to complications or relapse.
Fentanyl Detox
Fentanyl is a potent synthetic opioid medicine used to treat severe pain. It is similar to other opioids like oxycodone and morphine but is significantly more potent. Fentanyl addiction can be hazardous, as the drug is powerful and can cause respiratory depression, overdose, and death. Treatment for fentanyl addiction typically involves a combination of medication-assisted treatment, counseling, and support groups. This may include medications to manage withdrawal symptoms and cravings and counseling to address the psychological aspects of addiction.
Dilaudid Detox
Dilaudid is a potent prescription opioid medication used to manage severe pain. Detoxing from Dilaudid can be challenging and uncomfortable due to the potential for withdrawal symptoms, which can range from mild to severe. Treatment for Dilaudid detox typically involves managing withdrawal symptoms and providing support to help individuals cope with the process. This may include medications to contain symptoms such as anxiety, nausea, and pain and counseling or support groups to address the psychological aspects of addiction.
Methadone Detox
Methadone is a long-acting opioid drug beneficial to treat opioid addiction and relieving severe pain. It is often used as a replacement therapy for individuals struggling with opioid addiction to help manage withdrawal symptoms and cravings. As it is an opioid itself as well, methadone detox can help to safely stop the use of methadone while managing the symptoms of withdrawal.
World-class, Accredited, 5-Star Reviewed, Effective Addiction & Mental Health Programs. Complete Behavioral Health Inpatient Rehab, Detox plus Co-occuring Disorders Therapy.
CALL(844) 597-1011End the Addiction Pain. End the Emotional Rollercoaster. Get Your Life Back. Start Drug, Alcohol & Dual Diagnosis Mental Health Treatment Now. Get Free No-obligation Guidance by Substance Abuse Specialists Who Understand Addiction & Mental Health Recovery & Know How to Help.
Top 10 Opiate Withdrawal Help FAQs
-
How long does it take to detox from opiates?
The time it takes to detox from opiates is determined by the individual’s health, the type of opiates used, the duration and frequency of use, and other aspects such as overall health and any co-occurring medical or psychiatric conditions. Generally, the acute withdrawal symptoms of opiates typically peak within the first few days and begin to subside after about a week, although some symptoms may persist for several weeks. However, it can take longer for the brain and body to recover from the effects of long-term opiate use fully.
-
How long does opiate withdrawal last?
How long is opiate withdrawal? While the acute symptoms of opiate withdrawal typically subside within a week, some people may experience post-acute withdrawal syndrome (PAWS), lasting for weeks or even months. PAWS can include symptoms such as depression, anxiety, irritability, and difficulty sleeping. Withdrawal can be challenging and uncomfortable, and it’s best to seek professional medical help and support to manage the symptoms and ensure safe detoxification. Treatment options for opiate addiction may include medication-assisted treatment, counseling, and support groups.
-
Can you die from opiate withdrawal?
Can opiate withdrawal kill you? While opioid withdrawal itself is generally not fatal, it can be a complex and uncomfortable process, and there are certain risks and complications associated with the condition that can be potentially life-threatening. Medical professionals can provide appropriate treatment and medication to manage the symptoms and ensure a safe detoxification process. If you or someone you’re concerned with is experiencing opiate withdrawal, it’s vital to seek professional help immediately.
-
How to detox from opiates?
What helps with opiate withdrawal? Several evidence-based treatments and strategies can help manage the symptoms of opiate withdrawal and support recovery from opiate addiction. The most effective treatment approach for opiate withdrawal will depend on individual needs and preferences, and it’s best to work with an addiction treatment professional to develop a personalized treatment plan.
-
Does Klonopin help with opiate withdrawal?
Klonopin, also known as clonazepam, is a benzodiazepine medication that is sometimes used to manage the symptoms of opiate withdrawal. Benzodiazepines can help reduce anxiety, agitation, and insomnia, common symptoms of opiate withdrawal. However, using benzodiazepines for opiate withdrawal is generally not recommended as a first-line treatment. They can be habit-forming and have potential side effects, such as impaired coordination, dizziness, and drowsiness.
-
Does Gabapentin help with opiate withdrawals?
Can Gabapentin help with opiate withdrawal? Gabapentin is a medication that is sometimes used to manage the symptoms of opiate withdrawal, particularly for symptoms such as anxiety, insomnia, and restless legs from opiate withdrawal (RLS opiate withdrawal). While Gabapentin is not approved by the U.S. Food and Drug Administration (FDA) for the treatment of opiate withdrawal, several studies have shown that it can be effective in reducing opiate withdrawal symptoms and improving treatment outcomes. However, Gabapentin can have potential side effects, such as dizziness, drowsiness, and confusion, and can also be addictive if not used as directed. Therefore, it’s best to work closely with a healthcare professional to determine the appropriate dose and duration of Gabapentin treatment. Moreover, Gabapentin is not a substitute for other evidence-based treatments for opiate addiction, such as medication-assisted treatment (MAT) and counseling.
-
Does Buspirone help with opiate withdrawal?
Buspirone, also known as Buspar, is a medication that is sometimes used to manage the symptoms of opiate withdrawal, particularly for symptoms such as anxiety and agitation. However, while some studies have suggested that Buspirone may effectively reduce anxiety symptoms during opiate withdrawal, the evidence for its use in managing opiate withdrawal is limited. Furthermore, Buspirone is not approved by the U.S. Food and Drug Administration (FDA) for the treatment of opiate withdrawal, and it should not be used as a substitute for evidence-based treatments for opiate addiction, such as medication-assisted treatment (MAT) and counseling. MAT with medications such as methadone, buprenorphine, and naltrexone is effective in reducing opioid use, preventing relapse, and improving overall treatment outcomes. It’s best to consult an addiction treatment professional to determine the most appropriate treatment approach for your needs.
-
Can Clonidine help with opiate withdrawal?
Yes, Clonidine is a medication that is commonly used to manage the symptoms of opiate withdrawal. Clonidine works by reducing the activity of the sympathetic nervous system, which can help to reduce symptoms such as anxiety, agitation, and rapid heart rate, which are common during opiate withdrawal. Clonidine is often used with other medications, such as buprenorphine or methadone, to help manage opiate withdrawal symptoms. While Clonidine can help address some of the physical symptoms of opiate withdrawal, it is not a substitute for other evidence-based treatments for opiate addiction, such as medication-assisted treatment (MAT) and counseling.
-
What is a bridge device for opiate withdrawal?
The bridge device is a medical device that is used to help manage the symptoms of opiate withdrawal. It is a small electrical “bridge device opiate withdrawal tool” placed behind the ear and delivers electrical impulses to the cranial nerves responsible for transmitting pain and other sensations. The Bridge device is designed to provide non-narcotic relief from the symptoms of opiate withdrawal, including anxiety, insomnia, and cravings. It is typically part of a comprehensive treatment program that includes medication-assisted treatment (MAT), counseling, and other supportive therapies. While the Bridge device may be helpful for some people in managing the symptoms of opiate withdrawal, it is not a substitute for other evidence-based treatments for opiate addiction.
-
What are the COWS opiate withdrawal scale?
The Clinical Opiate Withdrawal Scale COWS is a standardized tool used by healthcare professionals to assess the severity of opiate withdrawal symptoms in people undergoing detoxification from opioids. The COWS clinical opiate withdrawal scale can help healthcare professionals determine the appropriate medication and support to manage opiate withdrawal symptoms. The tool can also help track withdrawal progress and adjust treatment as necessary. While the COWS can help assess and manage opiate withdrawal symptoms, opiate withdrawal scores should be used with other clinical assessments and interventions as part of a comprehensive therapy program for opioid addiction.
How Long Do Opiates Stay in Your System? How Long Do Opiates Stay in Urine, Blood, & Body?
How Long Do Opiates Stay in Your System? Brief Video Transcript.
Drugs in the opioid class are used to treat pain. Natural opioids, semi-synthetic opioids generated from natural opioids, and synthetic opioids produced in a lab are all referred to as opioids under the general term. A class of medications known as opioids contain opiates, which are organic byproducts of the poppy plant. The main difference is that “opiate” refers to the substances derived from the opium (poppy) plant. At the same time, “opioids” are all substances that interact with opioid receptors, including those created in the lab.
The length of time that opiates remain in your system varies depending on the type of opiate, the dosage, and the frequency of use. Generally, opiates can stay in your system for two to four days. However, heavier and chronic users may have residues in their system for up to seven days.
Opiates can be detected in the blood test for up to 24 hours and in the urine test for up to three days. Opiates can be detected in the hair follicles for up to 90 days. In chronic users, opiates can stay in the body for up to 30 days.
Opiates often have short half-lives, meaning their effects can linger for several hours even though they swiftly leave the body. However, Opioids can linger in a person’s bloodstream for several hours or days after the symptoms subside, depending on the substance used. Urine tests, one of the more common types of drug testing, can identify opioid usage for longer periods of time, often up to three to four days, and some tests can identify opioid use for up to three months.
Get FREE addiction treatment insurance check – https://welevelup.com/rehab-insurance/ If you or a loved one is struggling with opiates addiction or other substance use disorder(s), call for a FREE consultation 24/7 at (561) 678-0917
Experience Transformative Recovery at We Level Up Treatment Centers.
See our authentic success stories. Get inspired. Get the help you deserve.
Start a New Life
Begin with a free call to an addiction & behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up Treatment Center Network delivers recovery programs that vary by each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- World-class Amenities
- Licensed & Accredited
- Renowned w/ 100s 5-Star Reviews
We’ll Call You
Search We Level Up Opiate Detox, Mental Health Topics & Resources
Sources
[1] Dydyk AM, Jain NK, Gupta M. Opioid Use Disorder. [Updated 2022 Jun 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553166/
[2] Azadfard M, Huecker MR, Leaming JM. Opioid Addiction. [Updated 2023 Jan 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448203/
[3] Clinical Guidelines for Withdrawal Management and Treatment of Drug Dependence in Closed Settings. Geneva: World Health Organization; 2009. 4, Withdrawal Management. Available from: https://www.ncbi.nlm.nih.gov/books/NBK310652/
[4] Institute of Medicine (US) Committee on Opportunities in Drug Abuse Research. Pathways of Addiction: Opportunities in Drug Abuse Research. Washington (DC): National Academies Press (US); 1996. B, Drug Abuse Research in Historical Perspective. Available from: https://www.ncbi.nlm.nih.gov/books/NBK232965/
[5] Opiate and opioid withdrawal – U.S. Department of Health and Human Services National Institutes of Health Available from: https://medlineplus.gov/ency/article/000949.htm
[6] Prescription Opioids DrugFacts – National Institute on Drug Abuse (NIDA)
[7] Understanding the Opioid Overdose Epidemic – Centers for Disease Control and Prevention (CDC)
[8] Schiller EY, Goyal A, Mechanic OJ. Opioid Overdose. [Updated 2022 Sep 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470415/
[9] Narcotics (Opioids) – Drug Enforcement Administration (DEA)
[10] Risk Factors for Opioid Misuse, Addiction, and Overdose – U.S. Department of Labor


