Benzo Detox Timeline, Withdrawal Symptoms, Care & Treatment
Benzo detox should always be done under medical supervision, as withdrawal from benzodiazepines can be dangerous and potentially life-threatening. The process typically involves slowly tapering off the drug over several weeks or months, depending on the individual's needs and the severity of their addiction. Continue to read more about benzo detox.
By We Level Up | Editor Yamilla Francese | Clinically Reviewed By Lauren Barry, LMFT, MCAP, QS, Director of Quality Assurance | Editorial Policy | Research Policy | Last Updated: April 28, 2023
Benzo Detox Overview
Detox or detoxification is when a person abstains from or rids the body of unhealthy or toxic substances. The detoxification process for benzos has different stages. Many factors can affect the symptoms of benzo withdrawal, including how long you have used the drug, your dosage, and your health. Withdrawal symptoms of benzos usually start 24 hours after stopping the use of benzos, and they can last for an extended period.
Protracted benzo withdrawal is also common, when the persistent withdrawal symptoms can occur for weeks, months, or even years after an individual stops using benzodiazepines. These symptoms can vary widely but may include anxiety, depression, insomnia, muscle pain, fatigue, and cognitive difficulties. Early withdrawal from benzos symptoms is the process’s first part and can last a few days. You may experience anxiety and insomnia as your brain learns to work without drugs again.
If you want to begin your recovery from benzo addiction, the first step is to turn to a high-quality center for benzo detox. We Level Up can help you receive the medical assistance and skilled care needed to avoid the worst withdrawal symptoms associated with benzodiazepines.
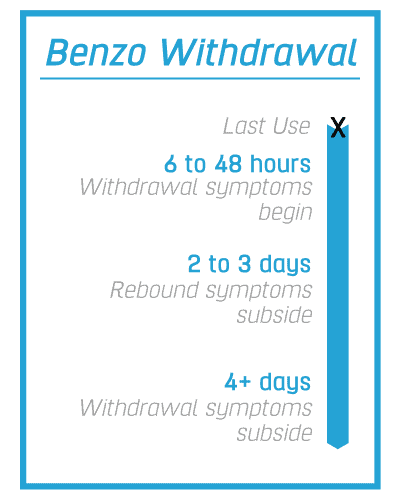
Benzo Withdrawal Timeline
The timeline for benzodiazepine withdrawal and the severity of withdrawal symptoms can be influenced by factors such as the length of time the individual has been using benzodiazepines, the dose they were taking, and their overall physical and mental health. Generally, benzodiazepine withdrawal follows a timeline with several distinct stages, including benzo withdrawal seizure timeline and the following phases:
| Acute withdrawal phase (0-4 weeks) | The first withdrawal stage typically lasts 1-4 weeks and is characterized by intense physical and psychological symptoms, including anxiety, insomnia, tremors, sweating, nausea, and irritability. |
| Early withdrawal phase (1-4 months) | After the acute withdrawal phase, symptoms may improve, but many individuals still experience residual symptoms, including fatigue, anxiety, depression, and difficulty concentrating. |
| Protracted withdrawal phase (4-12 months or longer) | Some individuals may experience a prolonged withdrawal phase, where symptoms continue for several months or even years after stopping benzodiazepines. These symptoms include anxiety, depression, sleep disturbances, and cognitive impairments. |
Benzo Withdrawal Symptoms
The detoxification procedure is a complex part of the recovery process from taking too much or using benzo for an extended period. You cannot begin treatment without removing the drug from your body, but this can lead to severe benzo withdrawals because your body has grown used to working with the drug.
Long-term use of benzos can cause your brain to stop making its own natural GABA chemicals, leading it to depend solely on the drug. Some of the most common benzodiazepine withdrawal symptoms can include the following:
- Nausea.
- Panic.
- Anxiety.
- Tremors.
- Headaches.
- Sweating.
- Muscle pain.
- Seizures.
- Palpitations.
- Fatigue.
- Sleeping disturbances.
You can risk developing benzo withdrawal syndrome if you attempt to stop using benzos rapidly and without medical assistance. This syndrome can cause:
- Seizures.
- Catatonia.
- Increased body temperature.
- Mania.
- Confusion.
- Violence and aggression.
- Suicidal ideation.
- Psychosis.
This is one of the most dangerous drugs to withdraw from, and dependence can develop in as little as a month of use, making medically professional benzo detox treatment essential. We Level Up is one of the leading benzo detox centers to help you begin your recovery process correctly.
How Long Do Benzo Withdrawal Symptoms Last?
Acute withdrawal symptoms of benzodiazepines can last anywhere from a few days to several weeks. However, some individuals may experience more prolonged withdrawal symptoms from benzos lasting for months or even years after stopping.
How long does benzo withdrawal last? The severity and timeline of withdrawal symptoms can also be influenced by how the drug is tapered or discontinued. A gradual tapering schedule that slowly reduces the dose of benzodiazepines over several weeks or months may help to minimize withdrawal symptoms and reduce the risk of protracted withdrawal.
Skip To:
Learn More:
- Benzos and Alcohol
- How Does Benzodiazepine Withdrawal Kill You?
- Benzodiazepine Withdrawal Psychosis
- Benzodiazepines Cardiac Side Effects
- Risks of Benzodiazepines, Uses, Side Effects, and Drug Abuse
- Benzos and Depression
- Benzos for Anxiety and Depression
- Benzo Addiction Treatment
- Prescription Drugs Addiction
- 10 Most Abused Prescription Drugs In The US
Benzodiazepine Drug Facts
What are Benzodiazepines?
Benzodiazepines, also known as benzos, first came into mainstream use in the 1960s and are still used in the treatment of many conditions, including the following:
- Anxiety disorders.
- Depression.
- Obsessive-compulsive disorder.
- Insomnia.
Benzodiazepines (benzos), such as Valium or Xanax, are central nervous system depressants that act similarly to alcohol. They cause users to feel sedated and relaxed, so doctors prescribe them for people with anxiety problems and sleep.
There are two different types of benzodiazepines, and these are hypnotic benzos and anxiolytic benzos. Hypnotic benzos, such as flurazepam and loprazolam, work best for sleeping problems. Anxiolytic benzodiazepine options work best for anxiety disorders. They include diazepam, lorazepam, and oxazepam.
Benzodiazepines can be highly addictive, making them appropriate only for short-term treatment. Chronic abuse of benzos for anxiety and depression often leads to benzo addiction.
Can you die from benzo withdrawal symptoms? Yes. If you or your loved one is undergoing or struggling with benzodiazepine addiction and withdrawal, seeking professional medical guidance and support is crucial. Symptoms of benzodiazepine withdrawal can escalate quickly and become life-threatening if left untreated.
Benzodiazepine Addiction & Overdose
Are benzodiazepines addictive ? Yes. Benzodiazepine drugs work by slowing down activity in the central nervous system. They recreate the effect of gamma-aminobutyric acid, or GABA, a natural chemical in the brain. GABA blocks specific brain signals affecting emotions, rational thought, memories, and essential functions. GABA also causes a calming effect on these parts of the brain.
However, one of the most significant risks of benzodiazepines and the reason to get into a benzo addiction treatment program is the high risk of overdose.
Some of the common signs of benzo addiction include the following:
- Blurred vision.
- Poor judgment.
- Impaired reasoning.
- Doctor shopping.
- Mood changes.
- Risk-taking behavior.
- Drowsiness.
- Being unable to stop using benzodiazepines.
People who use benzos can quickly grow a tolerance to the medication, which means they need more of it to produce the same calming effects. Using increasing amounts of benzos can put you at risk of overdosing.
Some of the symptoms of a benzo overdose include the following:
- Slurred speech.
- Confusion.
- Uncoordinated movement.
- Shallow breathing.
- Loss of consciousness.
- Extreme drowsiness.
Benzodiazepines Drug Fact Sheet. Publicly Made Available for Downloading by the DEA (Drug Enforcement Administration)
Download the below file for more information and facts about the risks of benzodiazepines. Benzodiazepine addiction is a condition that can develop when individuals use benzodiazepines in a way that is not prescribed by a healthcare provider or in amounts that are higher than recommended. Benzodiazepine addiction can be characterized by a compulsive pattern of drug use, despite harmful consequences such as physical, emotional, or social harm.

Get Your Life Back
Find Hope & Recovery. Get Safe Comfortable Detox, Addiction Rehab & Dual Diagnosis High-Quality Care.
Hotline(844) 597-1011Benzo Withdrawal Death Statistics
Withdrawal from benzo symptoms can include anxiety, insomnia, seizures, hallucinations, and delirium tremens. These symptoms can be severe and last several weeks, based on the individual’s usage and other factors. Delirium tremens can lead to death if left untreated.
It is crucial to get medical aid if you are experiencing benzos withdrawal symptoms, especially if you have a seizure history or other medical conditions. Your doctor or an addiction treatment professional may be able to provide pharmacotherapy or other treatments to manage your symptoms and help you safely withdraw from benzodiazepines.
12-48
The increased risk of using benzodiazepine to cause mortality begins at 12-48 months.
Source: NCBI
30.5 Million
Approximately 30.5 million people in the US use benzodiazepines, and according to the NIDA (National Institute on Drug Abuse), 17.1% of those people misuse the drug.
Source: NIDA
10%
According to the NIDA (National Institute on Drug Abuse), 10% of people undergoing a benzo detox process experience protracted withdrawal.
Source: NIDA
What Does Benzo Withdrawal Feel Like?
When does benzo withdrawal start? Acute withdrawal begins a few days after stopping the use of benzos. The worst withdrawal symptoms benzos can cause occur during this stage, including muscle spasms, anxiety, hallucinations, decreased appetite, trouble concentrating, and more.
Benzodiazepine withdrawal can be deadly because of potential seizures and other serious medical complications. Benzodiazepines act on the brain’s GABA receptors, which regulate the nervous system. When an individual stops taking benzodiazepines after long-term use or at high doses, the brain may become hyperactive and overexcitable, leading to seizures and other medical emergencies.
Seizures are the most serious potential complication of benzodiazepine withdrawal. Seizures can cause a loss of consciousness, convulsions, and even death. In addition to seizures, other possible complications of benzodiazepine withdrawal include delirium, psychosis, and suicidal thoughts. The severity of benzodiazepine withdrawal can vary depending on several aspects, including the dose and duration of benzodiazepine use, the individual’s overall health, and their history of addiction or substance use disorders. It’s essential to seek medical attention if you or someone you’re concerned with is experiencing symptoms of benzodiazepine withdrawal. A healthcare professional can examine the severity of the signs and provide appropriate treatment to help manage withdrawal and prevent potential medical complications.
Benzo Withdrawal Symptoms List
Benzo withdrawal symptoms can vary in severity and duration based on several factors, including the type of benzodiazepine, the dose, and the time of use. Here is a list of common symptoms and signs of benzo withdrawal:
Benzo Withdrawal Headache
Headaches are a common symptom of benzo withdrawal. Headaches can occur as part of the benzo withdrawal syndrome or as a separate symptom. The severity of headaches can vary from mild to severe and last several days or weeks. Several factors, including the following, can cause headaches during benzo withdrawal:
- Changes in brain chemistry.
- Increased tension in the muscles of the head and neck.
- Changes in blood flow to the brain.
- Headaches may also be caused by dehydration or changes in sleep patterns.
Benzo Withdrawal Insomnia
Insomnia is a common symptom of benzo withdrawal. Insomnia during benzodiazepine withdrawal can be caused by changes in brain chemistry, increased anxiety or agitation, and disruptions to sleep patterns.
Benzo Withdrawal Diarrhea
Diarrhea is one of the possible benzo withdrawal symptoms. Several factors, including changes in the gastrointestinal system and increased anxiety or stress, can cause diarrhea during benzo withdrawal.
It is crucial to monitor the frequency and severity of diarrhea during benzo detox and seek medical support if the symptoms persist or worsen. In some cases, diarrhea during benzo withdrawal can indicate a more severe underlying medical condition. Your doctor can provide additional treatment options or suggest further testing to identify any underlying causes of your symptoms.
Benzo Withdrawal Psychosis
Psychosis is a rare but possible symptom of benzo withdrawal. Psychosis during benzo withdrawal can manifest as hallucinations, delusions, disorientation, and paranoia. Psychosis during benzo withdrawal is more common in individuals with psychiatric disorders, such as schizophrenia or bipolar disorder.
If you experience symptoms of psychosis during benzo detox, it is crucial to seek medical attention immediately. Your doctor may recommend hospitalization for observation and treatment of your symptoms. Treatment for psychosis during benzodiazepine withdrawal may include medications such as antipsychotics, mood stabilizers, or benzodiazepines in some cases.
If you or someone you’re concerned with is experiencing symptoms of benzodiazepine withdrawal, it’s essential to seek medical attention. A healthcare professional can examine the severity of the signs and provide appropriate treatment, including medication-assisted therapy, counseling, or other forms of support. It’s crucial not to try to quit benzodiazepines cold turkey, as this can be dangerous and may lead to severe withdrawal symptoms. A healthcare professional can help you safely taper off the medication and manage withdrawal symptoms.
Protracted Benzo Withdrawal
Protracted benzo withdrawal, also known as post-acute withdrawal syndrome (PAWS), is a condition that occurs in some individuals who have undergone benzo withdrawal. PAWS refers to a prolonged period of withdrawal symptoms that can occur after the initial acute withdrawal phase has ended, typically lasting for several months to a year or more.
Some of the symptoms of prolonged withdrawal include the following:
- Tingling in arms and legs.
- Muscle twitches.
- Prolonged anxiety.
- Prolonged insomnia.
- Depression.
- Mood swings.
- Cognitive deficits.
Trying to go through this process alone can lead to severe symptoms and even increase your likelihood of using the drugs again to eliminate the withdrawal symptoms. Turning to medical benzo detox can help you avoid the worst of them. At We Level Up, we have a medical detox process that can keep you safe and help prevent uncomfortable withdrawal symptoms as you go through this stage of recovery.
Benzo Withdrawal Scale
Healthcare professionals use the benzo withdrawal scale to assess the severity of benzodiazepine withdrawal symptoms. The scale typically ranges from 0 to 67 and includes a list of symptoms that may occur during withdrawal. Some common symptoms of benzodiazepine withdrawal include anxiety, insomnia, agitation, irritability, tremors, sweating, and seizures.
Here is an example of a benzodiazepine withdrawal scale:
- 0 – No withdrawal symptoms.
- 1-10 – Mild withdrawal symptoms (mild anxiety, insomnia, agitation, irritability).
- 11-20 – Moderate withdrawal symptoms (moderate anxiety, insomnia, agitation, irritability, tremors).
- 21-30 – Moderate to severe withdrawal symptoms (severe anxiety, insomnia, agitation, irritability, tremors, sweating).
- 31-40 – Severe withdrawal symptoms (severe anxiety, insomnia, agitation, irritability, tremors, sweating, confusion).
- 41-50 – Very severe withdrawal symptoms (severe anxiety, insomnia, agitation, irritability, tremors, sweating, confusion, hallucinations).
- 51-60 – Extremely severe withdrawal symptoms (severe anxiety, insomnia, agitation, irritability, tremors, sweating, confusion, hallucinations, seizures).
- 61-67 – Life-threatening withdrawal symptoms (severe anxiety, insomnia, agitation, irritability, tremors, sweating, confusion, hallucinations, seizures, delirium).
Benzodiazepine withdrawal can be detrimental and should be managed by a healthcare professional with experience treating addiction and withdrawal. If you are experiencing symptoms of benzodiazepine withdrawal, seek medical attention immediately.
Alcohol and Benzo Withdrawal
With the proper use, benzodiazepines can help ease several conditions. As such, why are benzos used for alcohol withdrawal? Alcohol withdrawal syndrome (AWS) can occur when individuals who are physically dependent on alcohol stop drinking suddenly. AWS can cause a range of symptoms, including anxiety, insomnia, agitation, tremors, seizures, and delirium tremens (DTs), which can be life-threatening. Benzos can help manage these symptoms by reducing anxiety, promoting sleep, preventing seizures, and reducing the risk of DTs.

Benzo for alcohol withdrawal enhances the activity of GABA (gamma-aminobutyric acid), a neurotransmitter that helps regulate brain activity. GABA is inhibited by alcohol, and when alcohol is abruptly withdrawn, GABA activity can rebound, leading to overexcitation and the symptoms of alcohol withdrawal. Benzos enhance GABA activity, which can help reduce the symptoms of alcohol withdrawal.
However, while benzos can effectively manage the symptoms of alcohol withdrawal, they can also be addictive and cause withdrawal symptoms when use stops. Therefore, benzos for alcohol withdrawal should be used cautiously and under medical professionals’ guidance experienced in managing alcohol withdrawal. A tapering schedule is typically used to gradually reduce and eventually discontinue benzo use to prevent rebound symptoms and addiction.
Benzos for Opiate Withdrawal
Benzodiazepines are a type of drug that is generally used for anxiety, insomnia, and seizures. While they can be effective in managing some of the symptoms of opiate withdrawal, their use should be supervised by a medical professional.
Benzos can help alleviate anxiety, agitation, and insomnia symptoms during opiate withdrawal. However, they should be used cautiously because they can be addictive and cause various side effects, including drowsiness, confusion, and impaired coordination.
Moreover, benzodiazepines can be harmful when combined with opioids because they can increase the risk of respiratory depression, which can be life-threatening. Suppose you are considering using benzodiazepines to manage opiate withdrawal symptoms. In that case, it is crucial to do so under the direction of a healthcare professional who can monitor your progress and adjust your medication as needed. They can also help you to develop a comprehensive treatment plan that may include other medicines and therapies to help you manage your symptoms and stay on track with your recovery.
Get Help. Get Better. Get Your Life Back.
Searching for Accredited Drug and Alcohol Rehab Centers Near You?
Even if you have failed previously and relapsed, or are in the middle of a difficult crisis, we stand ready to support you. Our trusted behavioral health specialists will not give up on you. When you feel ready or just want someone to speak to about therapy alternatives to change your life call us. Even if we cannot assist you, we will lead you to wherever you can get support. There is no obligation. Call our hotline today.
(844) 597-1011Benzo Withdrawal Medication
Several medications can be used to manage the symptoms of benzodiazepine withdrawal. A healthcare professional can prescribe these medications, and should be used under their supervision to ensure safe and effective treatment.
While several medications can help manage some of the physical and psychological symptoms of benzo withdrawal, these medicines are not typically used as the sole treatment for benzodiazepine addiction. Additional therapies, such as counseling and support groups, may also support long-term recovery.
What helps with benzo withdrawal? Several medications may be used to manage the symptoms of benzo withdrawal, including the following:
- Gabapentin for benzo withdrawal.
- Gabapentin is a medication that is sometimes used to manage benzo withdrawal symptoms. Gabapentin is an anticonvulsant medication that affects the activity of certain neurotransmitters in the brain. It effectively addresses the symptoms such as anxiety, insomnia, and seizures during benzo withdrawal.
- Clonidine for benzo withdrawal.
- Clonidine is particularly helpful in managing symptoms such as high blood pressure and rapid heartbeat during benzo withdrawal. It can also help manage symptoms such as sweating, tremors, and anxiety.
- Flumazenil for benzo withdrawal.
- Flumazenil is a medication sometimes used to manage benzo withdrawal symptoms, but its use is controversial and not widely recommended. Flumazenil is a benzodiazepine antagonist that works by blocking the effects of benzodiazepines on specific receptors in the brain. It is effective in reversing the sedative effects of benzodiazepines in emergencies, such as when someone has overdosed on a benzodiazepine.
- Magnesium benzo withdrawal.
- Some studies have suggested magnesium for benzo withdrawal. Magnesium supplementation may help manage anxiety, insomnia, and muscle spasms. Magnesium can help regulate the activity of certain neurotransmitters in the brain, which can help manage benzo withdrawal symptoms.
- Hydroxyzine for benzo withdrawal.
- Hydroxyzine is an antihistamine with sedative effects and can help manage symptoms such as anxiety, agitation, and insomnia common during benzodiazepine withdrawal.
- Phenobarbital for benzo withdrawal.
- Phenobarbital is typically part of a comprehensive treatment plan for benzodiazepine withdrawal, which may include other medications and therapies such as clonidine, gabapentin, and counseling. Phenobarbital should not be used as the sole treatment for benzodiazepine addiction, and it is necessary to seek professional guidance and support when managing benzodiazepine withdrawal.
- Ketamine for benzo withdrawal.
- While there is some research on the use of ketamine for managing substance use disorders, including benzodiazepine addiction, the evidence is limited, and medical guidelines do not currently advise the use of ketamine for this purpose. Ketamine can have significant side effects, including hallucinations, disorientation, and confusion, and its long-term effects on the brain and body are not fully understood.
- L-Theanine for benzo withdrawal.
- L-Theanine is an amino acid generally found in tea leaves and certain mushrooms. While it has not been extensively studied for the management of benzo withdrawal symptoms, some research suggests that it may have anxiety-reducing effects and could potentially help manage symptoms of benzodiazepine withdrawal.
- Librium for benzo withdrawal.
- During benzodiazepine withdrawal, Librium can help manage symptoms such as anxiety, insomnia, and muscle spasms. It is generally used as a short-term treatment option, and the dosage and duration of treatment may vary based on the individual’s specific needs and circumstances.
First-class Facilities & Amenities
World-class High-Quality Addiction & Mental Health Rehabilitation Treatment
Rehab Centers TourRenowned Addiction Centers. Serene Private Facilities. Inpatient rehab programs vary.
Addiction Helpline(844) 597-1011Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Success Stories Across Our Network
- Low Patient to Therapist Ratio
- Onsite Medical Detox Center
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Personal Development Events
Benzo Withdrawal Treatment
How to help benzo withdrawal symptoms? The We Level Up benzo detox centers offer medication to help you go through the withdrawal process. Although no drug is specifically FDA-approved for the treatment of benzodiazepine dependence, medication for benzo withdrawal is used off-label to treat withdrawal symptoms or to manage the spectrum of symptoms that can arise during benzo withdrawal.
Some of the medications may include the following:
- SSRI antidepressants.
- Anticonvulsants.
- Beta-blockers.
For people with co-occurring mental health illnesses, it can be critical for medical professionals to distinguish between the symptoms that the disease causes and those that the addiction causes. When a person is diagnosed with a mental health disorder such as anxiety and depression, and drug or alcohol addiction, they are said to have co-occurring conditions. Though illnesses can exist separately from one another, when they coexist in the same individual, they generally cause the signs and symptoms of both disorders to be intensified. It is common for a person with co-occurring conditions to have more severe symptoms than a person with only one of the disorders.
What helps benzo withdrawal? Experts at We Level Up benzo detox centers can prescribe medications to manage the mental health disorder, address the addiction, and avoid developing new substance abuse. We always perform a thorough intake assessment at our centers, which allows us to identify co-occurring conditions, get a good idea of your physical and mental health, and prescribe the proper medications to help you as you detox.

Inpatient Benzo Detox Treatment
Inpatient benzo detox treatment is usually warranted when a person has been taking large doses of benzodiazepines for a long time, is suffering from polysubstance abuse, or experiencing co-occurring disorders.
The process starts with an intake assessment that can help us understand the severity of your addiction. We can then begin the detoxification process. During this process, you will have 24/7 monitoring and checkups throughout the day to ensure you are as comfortable as possible.
We will choose the best supplements for benzo withdrawal that sufficiently suit your needs and your health level, and we will perform many checks to ensure you can get the relief you need from the worst withdrawal symptoms.
Inpatient rehab centers, also known as residential rehab centers, offer a comprehensive approach to addiction treatment that can benefit individuals struggling with substance use disorders. Here are a few benefits of an inpatient rehab center:
- 24/7 Medical Care and Support: Inpatient rehab centers offer round-the-clock medical care and support, which is especially important during the initial stages of recovery when individuals experience withdrawal symptoms or other medical issues.
- Structured Environment: Inpatient rehab centers provide a structured environment free from triggers and distractions. This allows individuals to focus on their recovery without the stresses and distractions of daily living.
- Evidence-Based Treatment: Inpatient rehab centers offer evidence-based treatment modalities that are proven effective in treating addiction, such as cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and motivational interviewing.
- Peer Support: Inpatient rehab centers offer a supportive community of friends who are going through the same struggles. This can help individuals feel less alone and give them a sense of community and connection.
- Evidence-Based Care: Inpatient rehab centers often offer a range of holistic therapies and activities, such as yoga, meditation, art therapy, and exercise programs. These can help individuals address their addiction’s physical, emotional, and spiritual aspects and promote overall wellness.
- Aftercare Planning: Inpatient rehab centers help individuals develop a comprehensive aftercare plan to help them maintain their sobriety after they leave the program. This may include outpatient therapy, support groups, and other resources.
Benzo Detox Near Me
If you or someone you know is detoxing from benzos and looking for a center, there are several aspects to consider when selecting the right one. Here are some vital and significant things to look for benzo withdrawal help:
- Accreditation: Look for a detox center accredited by a recognized orgs., like the Joint Commission or the Commission on Accreditation of Rehabilitation Facilities. Accreditation assures that the facility meets specific standards of care and quality.
- Staff Qualifications: The staff at the detox center should be highly trained and qualified to provide medical and psychological care. Look for centers that have licensed physicians, nurses, therapists, and other healthcare professionals on staff. Benzo withdrawal stories and reviews can also help you decide.
- Treatment Options: Different detox centers may offer different treatment options, so finding one that provides the right level of care for your requirements is crucial. Some centers offer medication-assisted detox, while others focus on holistic or natural ways to ease benzo withdrawal.
- Location and Environment: The location and environment of the detox center can play a significant role in the success of your treatment. Look for a center that is in a safe and peaceful location, with comfortable accommodations and features that will make your stay as comfortable as possible.
- Aftercare Support: Detox is just the first step in the recovery process, so choosing a center offering aftercare support and resources to help you continue your sobriety is beneficial. Look for centers that provide counseling, support groups, and other resources to help you stay on track.
- Cost and Insurance: Detox centers can be expensive, so it’s essential to consider the cost and whether your insurance will cover it. Look for rehab centers that accept your insurance or offer financing options to help make addiction treatment more affordable.
Getting Help for Benzodiazepine Addiction
Benzo abuse can be devastating and affect all aspects of your life. If you have an addiction to benzodiazepines, reach out for help to get the medical detox assistance you need to begin your recovery correctly.
We Level Up benzo detox centers can get medical supervision that can help you get through your recovery process. We provide inpatient treatments to help those battling addiction and other mental health disorders and alums programs that can make it easier for you to maintain your sobriety after treatment.
Contact We Level Up today to begin your recovery. Benzo withdrawal symptoms may include insomnia, anxiety, and stress. However, these symptoms will likely subside or reduce as the body regulates through benzo detox.

Get FREE addiction treatment insurance check – https://welevelup.com/rehab-insurance/ If you or a loved one is struggling with benzodiazepines or other substance use disorder(s), call for a FREE consultation 24/7 at (561) 678-0917
World-class, Accredited, 5-Star Reviewed, Effective Addiction & Mental Health Programs. Complete Behavioral Health Inpatient Rehab, Detox plus Co-occuring Disorders Therapy.
CALL(844) 597-1011End the Addiction Pain. End the Emotional Rollercoaster. Get Your Life Back. Start Drug, Alcohol & Dual Diagnosis Mental Health Treatment Now. Get Free No-obligation Guidance by Substance Abuse Specialists Who Understand Addiction & Mental Health Recovery & Know How to Help.
Top 10 What Medications Help With Benzo Withdrawal? FAQs
-
How to ease benzo withdrawal?
The most crucial step in easing benzo withdraw symptoms is to taper off the drug gradually under the guidance of a healthcare provider. A slow and gradual taper can help to minimize withdrawal symptoms and reduce the risk of protracted withdrawal.
-
How to treat benzo withdrawal?
Everyone’s experience with benzodiazepine withdrawal is unique, and there is no one-size-fits-all approach to easing symptoms. Working closely with a healthcare provider knowledgeable about how benzo withdrawal symptoms come and go can help develop a personalized plan that meets your needs.
-
What are the supplements to avoid during benzo withdrawal?
Some supplements to avoid during benzodiazepine withdrawal include Kava, Valerian root, melatonin, St. John’s wort, and GABA supplements. Please speak to a healthcare provider before taking any supplements during benzodiazepine withdrawal, as they can help you determine which supplements are safe and appropriate for your individual needs.
-
Can you take CBD for benzo withdrawal?
More research is required to ensure the safety and efficacy of CBD (cannabidiol) for benzodiazepine withdrawal. Suppose you are considering using CBD during benzodiazepine withdrawal. In that case, it’s essential to talk to a knowledgeable healthcare provider about benzodiazepine withdrawal and CBD to help you make an informed selection based on your unique needs and health status.
-
Can you take trazodone for benzo withdrawal?
Whether or not trazodone is appropriate for benzodiazepine withdrawal depends on the individual’s needs and medical history. A healthcare provider who is knowledgeable about both benzodiazepine withdrawal and trazodone can help to determine whether trazodone is an appropriate treatment for benzo withdrawal and can provide guidance on how to use it safely and effectively.
-
What is benzo buddies withdrawal timeline?
“Benzo Buddies” is an online discussion and support group for individuals experiencing benzodiazepine withdrawal. Most members often talk about benzo buddies protracted withdrawal experiences. The withdrawal timeline can vary depending on the individual’s dosage, length of use, and other factors. Still, generally, the acute withdrawal phase lasts for several weeks to several months, while the post-acute withdrawal phase (PAWS) can last for several months to several years.
-
Is it adequate to take CIWA for benzo withdrawal?
The Clinical Institute Withdrawal Assessment for Alcohol (CIWA) is a validated tool commonly used to assess and monitor symptoms of alcohol withdrawal. Still, it is not designed explicitly for benzodiazepine withdrawal. While some of the symptoms of alcohol and benzodiazepine withdrawal may overlap, the severity and timeline of these symptoms can vary depending on the individual and the specific drug(s) involved.
-
What are the benefits of propranolol for benzo withdrawal?
Propranolol is a beta-blocker medication that is sometimes used off-label to help manage symptoms of benzodiazepine withdrawal, particularly symptoms related to anxiety and hyperarousal. Propranolol functions by blocking the effects of adrenaline on the heart and blood vessels, which can help to reduce heart rate, blood pressure, and other physical symptoms of anxiety. Whether propranolol is an appropriate treatment option for benzodiazepine withdrawal depends on the individual’s needs and medical history.
-
Is niacin for benzo withdrawal effective?
Niacin, also called vitamin B3, is a nutrient essential for various bodily processes, including energy production, DNA repair, and the maintenance of healthy skin, nerves, and digestion. While only a few have reported using niacin for benzodiazepine withdrawal, limited scientific evidence supports its effectiveness.
-
Is benzo withdrawal life threatening?
Can benzo withdrawal kill you? Yes. Withdrawal benzo experience can be a severe and potentially life-threatening condition in some cases, particularly for individuals who have been taking high doses of benzodiazepines or have been using these medications for an extended period. To withdraw from benzos, the symptoms can vary from mild to severe and may include insomnia, anxiety, irritability, tremors, seizures, hallucinations, and delirium.
Barbiturates Sedatives Hypnotics Effects, Warnings, Overdose Risks, Drug Facts, Detox & Treatment
Benzodiazepines and barbiturates are often compared because they are both central nervous system (CNS) depressants that can produce sedative, hypnotic, and anxiolytic effects. However, there are some critical differences between the two types of drugs.
While benzodiazepines and barbiturates are both CNS depressants that can produce similar effects, benzodiazepines are generally considered safer and less likely to cause severe adverse effects or overdose. However, both types of drugs can be addictive and cause withdrawal symptoms, so it’s crucial to use them exactly as prescribed and under the guidance of a healthcare provider.
Watch the video below to learn more about the dangers of barbiturate overdose.
Barbiturate Warnings Video Transcript
Welcome to the We Level Up treatment center video series. In today’s video, we will discuss What are Barbiturate Overdose Risks, Use, Effects, Withdrawal & Addiction Treatment Options?
What are barbiturates? Barbiturates are drugs used to treat anxiety, epilepsy, and sleeplessness. They are a type of central nervous system depressant that can potentially establish habits and be addictive. Overdosing on barbiturates can lead to respiratory depression, overdose, and even death.
Synthetic barbiturates drugs slow down the central nervous system. Barbiturates are used as sedatives or depressants, hypnotics, anticonvulsants, and as a component of anesthesia. Their effects range from mild sleepiness to coma. Barbiturates can also be used to relax patients before surgery. Barbiturates can make someone appear inebriated or drunk at relatively low doses.
Barbiturates are addictive. Those who take them develop a physical dependence on them. It may be fatal to stop using them (barbiturate withdrawal). Barbiturates’ ability to modify mood quickly leads to tolerance with continued use. Repeated usage increases the likelihood of developing severe poisoning as resistance to the fatal effects takes longer.
What are barbiturates used for?
Few substances are used in medicine today compared to the 1900s when barbiturates were first made available. In the past, barbiturates were frequently given to treat anxiety, sleeplessness, and depression. The National Institute of Health claims that Barbiturates are drugs that cause sleepiness and relaxation. A barbiturate overdose occurs when a patient consumes more of this medication than is typical or advised. Either by chance or by purpose, this may occur.
A barbiturate overdose poses a serious health risk. Therefore, it is no longer advised to use barbiturates as hypnotics or sedatives to ease daytime restlessness or insomnia brought on by everyday pressures. Due to these potentially fatal adverse effects, safer drugs have replaced barbiturates in many applications.
Barbiturates are mostly used today to treat severe and extreme cases of insomnia. These medications occasionally function as an adjuvant to anesthesia and aid in controlling epilepsy episodes. Barbiturates are classified as Schedule II, III, and IV depressants under the Controlled Substances Act, according to the US Drug Enforcement Agency.
What is the definition of barbiturates?
Like sleeping pills, barbiturates are defined as “downers.” They function by reducing the activity of your nervous system and brain. The individual feels at ease as a result. Barbiturates can impair memory and judgment. Barbiturates can also produce mood changes and make users furious, despondent, and exhausted. They are more harmful when misused because they are stronger than most sleeping pills. This medicine can cause tolerance in users, who then use it more frequently. When used frequently and for an extended period of time, they might weaken muscles, harm the liver, and damage bones.
Never mix two different medication types together. Taking barbiturates along with heroin or alcohol is extremely risky. Alcohol, heroin, and barbiturates all reduce brain and nervous system activity. Because the neurological system regulates respiration, combining these medicines increases the risk of a barbiturate overdose, which increases the likelihood that the user would cease breathing and pass away.
Experience Transformative Recovery at We Level Up Treatment Centers.
See our authentic success stories. Get inspired. Get the help you deserve.
Start a New Life
Begin with a free call to an addiction & behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up Treatment Center Network delivers recovery programs that vary by each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- World-class Amenities
- Licensed & Accredited
- Renowned w/ 100s 5-Star Reviews
We’ll Call You
Search We Level Up Benzo Detox, Mental Health Topics & Resources
Sources:
[1] Bounds CG, Nelson VL. Benzodiazepines. [Updated 2023 Jan 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470159/
[2] Edinoff AN, Nix CA, Hollier J, Sagrera CE, Delacroix BM, Abubakar T, Cornett EM, Kaye AM, Kaye AD. Benzodiazepines: Uses, Dangers, and Clinical Considerations. Neurol Int. 2021 Nov 10;13(4):594-607. DOI: 10.3390/neurolint13040059. PMID: 34842811; PMCID: PMC8629021.
[3] Griffin CE 3rd, Kaye AM, Bueno FR, Kaye AD. Benzodiazepine pharmacology and central nervous system-mediated effects. Ochsner J. 2013 Summer;13(2):214-23. PMID: 23789008; PMCID: PMC3684331.
[4] Brett J, Murnion B. Management of benzodiazepine misuse and dependence. Aust Prescr. 2015 Oct;38(5):152-5. DOI: 10.18773/austprescr.2015.055. Epub 2015 Oct 1. PMID: 26648651; PMCID: PMC4657308.
[5] Ait-Daoud N, Hamby AS, Sharma S, Blevins D. A Review of Alprazolam Use, Misuse, and Withdrawal. J Addict Med. 2018 Jan/Feb;12(1):4-10. DOI: 10.1097/ADM.0000000000000350. PMID: 28777203; PMCID: PMC5846112.
[6] Detoxification and Substance Abuse Treatment [Internet]. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2006. (Treatment Improvement Protocol (TIP) Series, No. 45.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK64115/
[7] Inanlou M, Bahmani B, Farhoudian A, Rafiee F. Addiction Recovery: A Systematized Review. Iran J Psychiatry. 2020 Apr;15(2):172-181. PMID: 32426014; PMCID: PMC7215253.
[8] Institute of Medicine (US) Committee on Opportunities in Drug Abuse Research. Pathways of Addiction: Opportunities in Drug Abuse Research. Washington (DC): National Academies Press (US); 1996. 8, Treatment. Available from: https://www.ncbi.nlm.nih.gov/books/NBK232966/
[9] Benzodiazepines and Opioids – National Institute on Drug Abuse (NIDA)
[10] NIDA. 2018, October 18. Research suggests benzodiazepine use is high while use disorder rates are low. Retrieved from https://nida.nih.gov/news-events/science-highlight/research-suggests-benzodiazepine-use-high-while-use-disorder-rates-are-low on 2023, April 28


