What is Fentanyl?
Is fentanyl an opioid? Yes. It is also sometimes used to treat patients with chronic pain who are physically tolerant to other opioids. In its prescription form, it is known by such names as Actiq®, Duragesic®, and Sublimaze®. This narcotic is a powerful synthetic opioid analgesic similar to morphine but is 50 to 100 times more potent. It is a Schedule II prescription drug, typically used to treat patients with severe pain or manage pain after surgery. Tolerance occurs when you need a higher and/or more frequent amount of a drug to get the desired effects.
The illegally used narcotic most often associated with recent overdoses is made in labs. This synthetic opioid is sold illegally as a powder, dropped onto blotter paper, put in eye droppers and nasal sprays, or made into pills that look like other prescription opioids. Synthetic opioids are now the most common drugs involved in drug overdose deaths in the United States. Synthetic opioids are substances synthesized in a laboratory that act on the same targets in the brain as natural opioids (e.g., morphine and codeine) to produce analgesic (pain relief) effects.
Medical Uses
Fentanyl is a powerful synthetic opiate analgesic. It is considered to be 50- to 100 times more powerful than morphine and is often used to treat patients with severe pain. When taken as prescribed, it can be a safe and effective treatment option. However, because of its potency, it can be misused and abused and has a high risk of addiction and overdose. When misused or abused, fentanyl can cause serious and potentially fatal side effects.
Why do people take fentanyl? This narcotic, a potent opioid agonist, was developed in the 1950s to fill a need for potent and rapid analgesia. Because of these features, It is commonly used to treat chronic cancer pain or in anesthesia.
When prescribed by a doctor, it can be given as a shot, a patch on a person’s skin, or as lozenges that are sucked like cough drops.
When prescribing painkillers, healthcare providers can:
- Recognize that individuals are at risk of a prescription painkiller overdose.
- Follow guidelines for responsible prescribing, including screening and monitoring for substance abuse and mental health problems.
- Use prescription drug monitoring programs to identify patients who may be improperly obtaining or using prescription painkillers and other drugs.
Prescription opioids are powerful pain-reducing medications with benefits and potentially serious risks. However, too many Americans have been impacted by the serious harms associated with these medications, and despite ongoing efforts, the scope of the opioid crisis continues to grow.
Fentanyl Side Effects
Like heroin, morphine, and other opioid drugs, it works by binding to the body’s opioid receptors, which are found in areas of the brain that control pain and emotions. After taking opioids many times, the brain adapts to the drug, diminishing its sensitivity and making it hard to feel pleasure from anything besides it. When people become addicted, drug seeking and use take over their lives. Side effects of fentanyl may include the following:
- Extreme happiness
- Drowsiness
- Nausea
- Confusion
- Sedation
- Constipation
- Sedation
- Problems breathing
- Unconsciousness
How long does fentanyl stay in your system? It has a half-life of 7 hours, and experts usually agree that it takes 4 to 5 half-lives for a drug to be cleared from your body (which calculates to 35 hours). However, the actual length of time or how long does fentanyl stay in your system depends on what dose you took and how you took it (for example, by injection, via a patch, or orally), if you have been taking it for a long time, your weight, what other medications you take, and if you have kidney or liver disease.
Someone using the drug once or twice can process and remove opioids much faster than someone who uses high doses consistently.
Rainbow Fentanyl Pills Dangers
Rainbow fentanyl pills are very dangerous opioid drugs illicitly produced by mixing non-pharmaceutical fentanyl with other substances. Rainbow fentanyl pills are up to 10 times stronger than regular Fentanyl and can quickly cause a fatal overdose. As with other forms of Fentanyl, rainbow fentanyl pills should be avoided.
Rainbow fentanyl pills are often disguised as varieties of street drugs, like cocaine, MDMA, and other opioids. Users are often unaware of what they buy and consume and subsequently overdose. Rainbow fentanyl pills can also be made in tablet form, with each pill containing up to 50 mg of the drug, which is five times the lethal dosage for people who do not have a tolerance for opioids.
What does a Rainbow Fentanyl Overdose Looks Like?
A rainbow fentanyl overdose looks like intense:
- Dizziness & confusion.
- Cardiac arrest.
- Respiratory depression.
- And possible death.
A rainbow fentanyl overdose looks like seizures, comas, and even death in severe cases. It is important to seek medical attention immediately if someone is suspected of taking rainbow fentanyl.

Rainbow fentanyl pills are extremely potent and lethal, even in small doses. Too many rainbow fentanyl pills can lead to tolerance, addiction, and abuse. It is critical to recognize the signs of a fentanyl overdose and to get medical help as soon as possible.
Other rainbow fentanyl overdose symptoms can include intense stomach pain, clamy skin, pinpoint pupils, slow shallow breathing, blue or purple lips with loss of consciousness, and coma. If left untreated, a rainbow fentanyl overdose could be lethal.
Fentanyl Withdrawal Symptoms
Fentanyl withdrawal symptoms can vary depending on the individual and how much fentanyl one has been using. Common withdrawal symptoms include anxiety, restlessness, muscle aches, nausea, vomiting, sweating, fever, and insomnia. Other withdrawal symptoms can include depression, suicidal thoughts, flashbacks, hallucinations, and an increased heart rate. It is important to seek medical help if you or a loved one are experiencing these symptoms.
How long does fentanyl stay in your system? When people immediately stop using this narcotic within their system, they will experience particular body changes that may be extremely uncomfortable or painful. These withdrawal symptoms impact a person’s recovery as they may use the drug again to address their severe pain or discomfort. Withdrawal may take more than 2 weeks, with people usually getting better after a few days from the worst case of their symptoms.
Fentanyl Withdrawal Timeline
It is also important to remember that although fentanyl is an incredibly powerful opioid, it is possible to manage withdrawal symptoms and achieve recovery with treatment. Having friends and family around who can support and encourage recovery is important. A doctor should be consulted to manage any withdrawal-related medical issues adequately. Seeking professional help to manage opioid use and address underlying issues is the best way to overcome fentanyl addiction and withdrawal.
The fentanyl withdrawal timeline can vary based on the severity of addiction, length of use, and individual’s body chemistry. Generally, withdrawal symptoms appear 8-24 hours after the last use and can last anywhere from 3-14 days, depending on the individual. The most intense symptoms usually last up to 5 days and then start to taper off.
Withdrawal from fentanyl can cause both physical and psychological symptoms. On the physical side, symptoms can include excessive sweating, insomnia, body aches and pains, tremors, nausea, abdominal cramps, and intense cravings for the drug. Psychological symptoms may include depression, anxiety, flashbacks, mood swings, irritability, and even suicidal thoughts or feelings. It’s important to note that different people experience different symptoms, which may last for different lengths of time.
Dangers of Overdose on Fentanyl
DEA warns of brightly colored fentanyl, called rainbow fentanyl, most particularly aimed at young adults who buy fentanyl online. A person can accidentally overdose on fentanyl in candy, fentanyl rainbow pills, purple fentanyl, fentanyl-laced marijuana, and even fentanyl on dollar bills. An overdose occurs when a drug produces serious adverse effects and life-threatening symptoms. When people experience fentanyl overdose symptoms, their breathing can slow or stop. This can decrease the amount of oxygen that reaches the brain, a condition called hypoxia. Hypoxia can lead to a coma, permanent brain damage, and death.
What is Rainbow Fentanyl?
Rainbow fentanyl is an illicit drug of various colored substances intended to appeal to younger drug users by making it look like candy. The colors don’t indicate the potency or content of the drug; rainbow fentanyl can be highly toxic and dangerous even when it appears harmless.
Many elements may influence how long does fentanyl stay in your system and how your body interacts with a certain medication or other substances, or even affect detection time. This is more apparent in narcotic substances used recreationally or medically by users.

Rainbow fentanyl is typically cut with other substances such as caffeine, over-the-counter drugs, and even rat poison. This increases its potency and is dangerous since these substances are not meant to be ingested. In addition to being potentially deadly, rainbow fentanyl is also highly addictive. The high from rainbow fentanyl is short-lived, but when users cannot find their next dose, they can intensify their cravings for more of the drug.
Skip To:
Learn More:
- Fentanyl Detox
- Fentanyl and Alcohol
- Fentanyl Rehab
- Withdrawal From Fentanyl
- Fentanyl Withdrawal Timeline
- Effects of Fentanyl Abuse
- Fentanyl Abuse Signs
- Fentanyl Patch Abuse
- What Does Fentanyl Taste Like?
- Fentanyl Addiction
Fentanyl Overdose Symptoms Risks
Fentanyl overdose symptoms can be difficult to recognize since they are often similar to those of other narcotics. The most common symptoms of a fentanyl overdose include:
- Shallow breathing
- Blue nails and lips
- Dizziness and confusion, disorientation
- Extreme sleepiness
Other rainbow fentanyl overdose symptoms may include nausea, vomiting, and constipation. In severe cases, Fentanyl overdose symptoms can result in coma and even death. Fentanyl overdoses can be life-threatening and require immediate medical attention. Signs of a fentanyl overdose include: shallow breathing, pinpoint pupils, muscle rigidity, drowsiness, confusion, lethargy, and loss of consciousness. It is important to call 911 immediately if an overdose is suspected. Additionally, staying informed on the various types of drugs on the street and only purchasing from reputable dealers is vital.
If a person suspects they or someone else may have overdosed on fentanyl, it is important to move to a safe location and avoid going alone. If available, having a friend or family member with the person can help provide support. Furthermore, it is important to keep the person calm, as agitation can worsen the effects of an overdose.
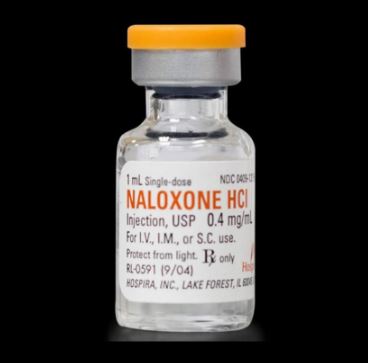
Nearly 50,000 people died from an opioid-involved overdose in 2019. One study found that bystanders were present in more than one in three overdoses involving opioids. With the right tools, bystanders can act to prevent overdose deaths. Anyone can carry naloxone, give it to someone experiencing an overdose, and potentially save a life.
Carrying naloxone is no different than carrying an epinephrine auto-injector (EpiPen) for someone with allergies. It provides an extra layer of protection for those at a higher risk for overdose.
There are several risk factors for opioid overdose. These include:
- Having an opioid use disorder;
- Taking opioids by injection;
- Resumption of opioid use after an extended period of abstinence (e.g. following detoxification, release from incarceration, cessation of treatment);
- Using prescription opioids without medical supervision;
- High-prescribed dosage of opioids (more than 100 mg of morphine or equivalent daily).
- Using opioids in combination with alcohol and/or other substances or medicines that suppress respiratory function, such as benzodiazepines, barbiturates, anesthetics, or some pain medications; and
- Having concurrent medical conditions like HIV, liver or lung diseases, or mental health conditions.
Males, people of older age, and people with low socio-economic status are at higher risk of opioid overdose than women, people of young age groups, and people with higher socio-economic status.
How long does fentanyl stay in your system? With tablets, the amount of time it takes to stop feeling the effects depends on the dose. Larger doses take longer to wear off. However, whether this drug shows up on a drug test differs from whether you feel the effects. It doesn’t matter what method you’re using; lozenges, patches, and IV, these narcotics can all show up on drug tests at the same time after use.
Fentanyl Overdose Amount
How does fentanyl kill you? Dealers are reported to execute fentanyl poisoning by producing folded dollar bills fentanyl, rainbow fentanyl lego box, fentanyl laced money, and fentanyl in marijuana. In any form, it is a deadly drug found in illicit street drugs. Addicts who buy fentanyl lethal doses illegally or on the street frequently misuse it.
How much fentanyl will kill you? According to test findings, 2 out of every 5 confiscated fake pills have deadly levels, which the DEA classifies as 2 mg of fentanyl structure. However, because lab-produced fentanyl dosing and its analogs come in so many variations and are frequently mixed with other illegal substances, it is exceedingly challenging to pinpoint the exact dosage that would cause death. Death following opioid overdose is preventable if the person receives basic life support and the timely administration of the drug naloxone. Naloxone is an antidote to opioids that will reverse the effects of an opioid overdose if administered in time. Naloxone has virtually no effect on people who have not taken opioids.
In-depth Signs and Symptoms of Fentanyl Overdose
An overdose from fentanyl symptoms looks very distinct from a normal high. When high on opioids, they often look very relaxed, nod off to sleep effortlessly, and slur their speech. But, in an overdose, someone looks more unconscious than just comfortable. Like other opioids, this potent opioid produces predictable overdose signs and effects. So the signs are the same whether someone overdoses on heroin, morphine, or dosage for fentanyl patch, fentanyl overdose dollar bill laced or fentanyl candy pills. Someone who has overdosed on it can have one or more of the following symptoms:
- Breathing that is slow, shallow, erratic, or completely stopped
- Severe lethargy, difficulty waking, or unconsciousness
- Small, “pinpoint” pupils
- Weak pulse, which might feel either slow or fast
- Vomiting
- Choking or gurgling sounds with breathing
- A limp or lifeless look
- A pale look
- Skin that feels cold and clammy
- Blue lips and fingernails
Opioid overdoses are destructive because slowed breathing can reduce oxygen to the brain and other organs. And, without oxygen, the body can’t survive for long. Even with an immediate response, someone can suffer long-term brain damage.
A fentanyl overdose can be difficult to manage, so it’s important to get medical help as soon as possible if you or someone you know might be experiencing an overdose. Treatment is often centered around managing the symptoms, including providing oxygen and intravenous fluids, using reversal medications, or using other medications to diminish the effects of fentanyl. It is also important to seek professional help for counseling and an opioid treatment program to prevent future overdoses.
How Long Does Fentanyl Stay in Your System?
When detoxing from this potent opioid, it’s natural to wonder how long does fentanyl stay in your system completely. Fentanyl can remain in your system for up to 72 hours after a single dose. However, the time it remains in your system varies, depending on the dose, your metabolism, and other factors. How long does fentanyl stay in your system? The drug can be detected in a urine sample for up to five days, in a blood sample for 24 to 48 hours, and in hair follicles for up to 90 days.
The amount of time that opioids stay in your system is determined by several factors, including the specific opioid, the amount of that opioid that was consumed, the individual’s history of opioid use, the individual’s medical history, weight, gender, and others. However, some general guidelines can be used to determine how long an opioid will be detectable in the body.
Employers frequently take the precaution of drug testing potential employees to ensure they will be dependable and productive. Drug testing is also often employed in several other situations, such as those involving competitive athletics, parole, child custody battles, and workmen’s compensation. Contrary to common belief, not all tests examine the same substances or collect pee. Some testing techniques can identify drug usage many months before the test date.
Fentanyl Drug Test
There are several types of fentanyl drug tests available. These include urine, saliva, hair, and blood tests. Each test is designed to detect different concentrations of fentanyl and its metabolites in different biological samples. Depending on the type of test and when it needs to be done, different specimens may be collected, stored, and analyzed differently to ensure accurate results.
Blood tests for fentanyl are usually performed in a laboratory setting and may require a healthcare professional to provide the necessary sample. This type of test is very accurate and can detect the presence of fentanyl and its metabolites in the blood up to 48 hours after the initial exposure. Saliva tests can detect fentanyl and its metabolites up to 12 hours after the initial exposure and provide a faster, more cost-effective option than a blood test.
Fentanyl Urine Test
A fentanyl urine test is typically administered as part of a standard panel of drug tests and is used to identify drug use that may be occurring. However, due to the short half-life of fentanyl, this type of test is not a reliable way to detect recent use.
While fentanyl urine tests are commonly used to detect current drug use, they are unreliable. Fentanyl has a half-life of only three to four hours, meaning that a urine test may not detect any use outside of that time frame. Additionally, due to the potency of fentanyl, other drugs may be detected as substitutions for fentanyl, resulting in a false positive result. Confirming any detections by other means is essential to ensure accurate and reliable results.
How long does fentanyl stay in your system? The best way to know whether this drug is still in your system is by taking a drug test. If you’re in active treatment, searching for a job, or reporting to a parole board, you might be required to take regular drug tests. The types of drug tests for opioids include hair, saliva, blood, and urine tests.
Fentanyl Drug Test FAQs
-
Does fentanyl show up on a drug test?
Yes, fentanyl can show up on a drug test. It may be detected in urine, blood, or saliva, depending on the test type used. The sensitivity of a drug test can vary, but generally, fentanyl can be detected in a drug test for up to 48 hours after use.
-
What does fentanyl show up as on a drug test?
Fentanyl typically appears on a drug test as fentanyl or metabolites of fentanyl.
-
How to pass a drug test for fentanyl?
The best way to pass a drug test for fentanyl is to stop using it and allow enough time for it to be eliminated from your system naturally. Additionally, drinking plenty of water can help accelerate the process.
Fentanyl Patches
Fentanyl patches relieve severe pain in people who are expected to need pain medication around the clock for a long time and who cannot be treated with other medications. Fentanyl is in a class of medications called opiate (narcotic) analgesics. It works by changing how the brain and nervous system respond to pain. Unfortunately, the regular use of opioids—even as prescribed by a doctor—can also lead to dependence. And when misused, opioid pain relievers can lead to addiction, overdose incidents, and deaths.
Fentanyl Patch Side Effects
Can fentanyl be absorbed through the skin by touching it? Yes. It can be absorbed into the body via inhalation, oral exposure or ingestion, or skin contact.
Fentanyl patches may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- Headache
- Mood changes
- Feeling cold
- Drowsiness
- Depression
- Difficulty falling asleep or staying asleep
- Uncontrollable shaking of a part of the body
- Pain, burning, tingling, or numbness in the hands or feet
- Dry mouth
- Stomach pain
- Indigestion
- Back pain
- Difficulty urinating
- Itching
- Skin irritation, redness, itching, or swelling in the area where you wore the patch
Some side effects can be serious. If you experience any of these symptoms or those listed in the IMPORTANT WARNING section, call your doctor immediately:
- Changes in heartbeat
- Agitation, hallucinations (seeing things or hearing voices that do not exist), fever, sweating, confusion, fast heartbeat, shivering, severe muscle stiffness or twitching, loss of coordination, nausea, vomiting, or diarrhea
- Nausea, vomiting, loss of appetite, weakness, or dizziness
- Inability to get or keep an erection
- Irregular menstruation
- Decreased sexual desire
- Chest pain
- Seizure
- Rash
- Hives
- Swelling of the eyes, face, mouth, tongue, throat, arms, hands, feet, ankles, or lower legs
- Hoarseness
- Difficulty breathing or swallowing
Fentanyl Patch Overdose Symptoms
While using these narcotic patches, you should talk to your doctor about having a rescue medication called naloxone readily available (e.g., at home or the office). Naloxone is used to reverse the life-threatening effects of an overdose. It works by blocking the effects of opioids or opiates to alleviate dangerous symptoms caused by high levels of narcotics in the blood. Your doctor may also prescribe you naloxone if you live in a household with small children or someone who has abused street or prescription drugs.
You should ensure that you and your family members, caregivers, or those who spend time with you know how to identify an overdose, how to use naloxone, and what to do until emergency medical help arrives. Your doctor or pharmacist will show you and your family how to use the medication. Ask your pharmacist for the instructions or visit the manufacturer’s website to get the instructions.
If symptoms of an overdose happen, a friend or family member should give the first dose of naloxone, call 911 immediately, stay with you, and watch you closely until emergency medical help comes. Your symptoms may return within a few minutes after you receive naloxone. If your symptoms return, the person should give you another dose of naloxone. Further doses may be given every 2 to 3 minutes if symptoms return before medical help arrives. Symptoms of overdose may include the following:
- Difficulty breathing
- Slow or shallow breathing
- Extreme sleepiness or tiredness
- Difficulty walking, thinking, and talking
- Small, pinpoint pupils (black circles in the center of the eye)
- Faintness
- Dizziness
- Confusion
- Unable to respond or wake up
Fentanyl Patch Abuse
Misuse of a drug can come in the form of taking it more often than prescribed, taking it in a greater amount than prescribed, taking it for a reason other than prescribed, or taking it without a prescription. For instance, someone prescribed one patch every 72 hours and applies a new one after just 60 hours is misusing it. However, if they have applied a new patch for a legitimate reason, like to manage their pain, this would be characterized as accidental misuse—which seems innocent but is incredibly hazardous.
Opioids are extremely potent, and someone using an opioid patch can suffer from an overdose even when taking a relatively low dose. Tolerance amplifies the risk of an overdose because it can lead to a person self-administering more of the drug by changing their patch more often or wearing more than one, which can overwhelm their system even if they aren’t actively feeling pain relief or other effects from the patch.
As mentioned earlier, fentanyl is a synthetic opioid 100 times stronger than morphine. Due to its powerful opioid properties, the opioid diversion of this drug for misuse is a problem. Fentanyl is added to heroin to increase its potency or is disguised as highly potent heroin. Many users believe they are purchasing heroin, but it has been adulterated with fentanyl – which often results in overdose deaths.
Fentanyl Facts
What Does Fentanyl Look Like?

How does fentanyl make you feel? It is an opioid used as a prescription painkiller, usually in the form of a patch or a pill. It can also be used in anesthesia. However, similar to other opioid analgesics, it produces effects such as relaxation, euphoria, pain relief, sedation, confusion, drowsiness, dizziness, nausea and vomiting, urinary retention, pupillary constriction, and respiratory depression.
Fentanyl Warnings
This opioid may cause a serious allergic reaction called anaphylaxis. Anaphylaxis can be life-threatening and requires immediate medical attention. Call your doctor right away if you or your child have a rash, itching, hoarseness, trouble breathing, trouble swallowing, or any swelling of your hands, face, or mouth while you are using this medicine.
Do not use too much of this narcotic or use it more often than your doctor tells you to. This can be life-threatening. Symptoms of an overdose include extreme dizziness or weakness, slow heartbeat or breathing, seizures, trouble breathing, and cold, clammy skin. Call your doctor right away if you notice these symptoms.
Do not take other medicines unless they have been discussed with your doctor for fentanyl interactions. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
There is no way to tell exactly or 100% how long does fentanyl stay in your system and how long fentanyl will be detectable in drug tests. The only way to pass a drug test is to stop using drugs. Treatment can help.
Facts About Fentanyl
Fentanyl Pronunciation: fen · tuh · nuhl
Fentanyl in Spanish: Fentanilo
Fentanyl Street Names: Apace, China Girl, China Town, China White, Dance Fever, Goodfellas, Great Bear, He-Man, Poison, and Tango & Cash
How strong is fentanyl? It is a synthetic opioid that is up to 50 times stronger than heroin and 100 times stronger than morphine. It is a major contributor to fatal and nonfatal overdoses in the U.S.
To define fentanyl, there are two types of this drug:
- Pharmaceutical fentanyl and
- Illicitly manufactured fentanyl
Both are considered synthetic opioids. Pharmaceutical fentanyl is prescribed by doctors to treat severe pain, especially after surgery and for advanced-stage cancer.
However, most recent cases of fentanyl-related overdose are linked to illicitly manufactured opioids, which are distributed through illegal drug markets for their heroin-like effect. It is often added to other drugs because of its extreme potency, which makes drugs cheaper, more powerful, more addictive, and more dangerous. [4] Learn more about “What does fentanyl feel like?” and opioid fentanyl addiction-related topics below:
DEA Counterfeit Pills Fact Sheet Publicly Made Available for Substance Use Disorder Awareness
How to make fentanyl? Illicitly manufactured fentanyl has been specially designed to be more powerful than other opioids like heroin. This makes it a popular choice for drug dealers who want to dilute their product without their customers realizing it.
Top 5 Fentanyl Pills FAQs
-
Where to buy fentanyl test strips?
Look for organizations in your city or state that distribute fentanyl strips. In April 2021, CDC and the Substance Abuse and Mental Health Services Administration (SAMHSA) announced that federal funding could be used to purchase FTS.
-
How long does fentanyl last?
It is a short-acting opioid, like heroin. It will create effects and stay in the body less than long-acting opioids, like methadone. The effects can last anywhere from 30 minutes to 3 days.
-
What schedule is fentanyl?
Fentanyl Schedule II prescription drug, is typically used to treat patients with severe pain or to manage pain after surgery. However, schedule II drugs, substances, or chemicals are defined as drugs with a high potential for abuse.
-
Can you smoke fentanyl?
Smoking fentanyl is growing more common. Across the country, fentanyl has rapidly become a primary opioid in the illicit drug supply.
-
What does fentanyl smell like?
Fentanyl doesn’t have a smell when you sniff it. It tastes like you’re sniffing Tylenol. Although many illegal dealers produce fentanyl sweet tarts, candy fentanyl, brightly colored fentanyl pills with added flavoring, fentanyl in weed, fentanyl lollipop, fentanyl in skittles or fentanyl in candy boxes, and fentanyl in cocaine and other illicit drugs. Making it harder to detect if the drugs or substances you are taking are laced.
Fentanyl Overdose Statistics
According to the DEA, 107,375 people in the United States died of drug overdoses and poisonings in the 12-month period ending in January 2022. A staggering 67% of those are reported fentanyl deaths in 2022. [5] If you or someone you know is at increased risk for opioid overdose, especially those struggling with opioid use disorder (OUD), you should carry naloxone and keep it at home. Naloxone is a life-saving medication that can reverse an overdose of opioids—including heroin, fentanyl short-acting or long-acting, and prescription opioid medications—when given in time.
People taking high-dose opioid medications (greater or equal to 50 morphine milligram equivalents per day) prescribed by a doctor, people who use opioids and benzodiazepines together, and people who use illicit opioids like heroin should all carry naloxone. Because you can’t use naloxone on yourself, let others know you have it in case you experience an opioid overdose.
What is rainbow fentanyl pills? DEA reported a rainbow fentanyl drug bust that illustrates drug traffickers’ latest marketing tactics to attract the public while deceiving them about the potentially lethal contents of pills sold on the street. There are fentanyl news and fentanyl bust about “fentanyl in Halloween candy warning” and “rainbow fentanyl Halloween candy.” These are reported cases of fentanyl found in candy. The Fentanyl crisis is an epidemic that now affects adults and children.
Fentanyl deaths per year are discussed every fentanyl awareness day, which happens on the first week of the month of May. This day aims to amplify nationwide efforts to increase awareness and decrease demand for fentanyl, a highly addictive synthetic opioid that continues to drive the overdose epidemic.
70,029
The new data show overdose deaths involving opioids increased from an estimated 70,029 in 2020 to 80,816 in 2021.
Source: CDC, Fentanyl Deaths 2021
53,480
The fentanyl category of opioids accounted for 53,480 preventable deaths in 2020, representing a 59% increase over the 33,725 total in 2019.
Source: DEA
40%
In nearly 40% of fentanyl overdose deaths 2021, someone else was present. Having naloxone available allows bystanders to help with a fatal overdose and save lives.
Source: NIDA
Fentanyl Overdose Symptômes
Canada’s street drugs have become tainted with powerful opioids, such as rainbow fentanyl. This is leading to a high rate of overdoses and deaths. Fake pills are being produced using unknown amounts of fentanyl. Many are searching for “fentanyl overdose symptoms,” as the opioid crisis is growing in Canada, driven by both illegal and prescription opioid use. Fentanyl and analogs appear to be fuelling the rise in opioid-related deaths.
- This crisis is devastatingly impacting the health and lives of Canadians, their families, and communities nationwide. In 2016 alone, there were 2861 opioid-related deaths and 16 daily hospitalizations.
- While the opioid crisis has affected every region of the country, western Canada (British Columbia and Alberta) and the northern territories (Yukon and Northwest Territories) have experienced the highest burden.
- Nationally, the most apparent opioid-related deaths occurred among males (74%); individuals between 30 and 39 years of age accounted for the greatest proportion (28%).
- Evidence reveals that this crisis is not restricted to opioids; 82% of apparent opioid-related deaths from January 2016 to June 2017 also involved one or more non-opioid substances.
Emergency Department Care
The ABCDE protocol must be followed when a patient presents to the emergency department with any drug overdose. In some cases, airway control has been obtained by emergency medical personnel at the scene. Still, if there is any sign of respiratory distress or failure to protect the airways in an un-intubated patient with a morphine overdose, one should not hesitate to intubate. Next, immobilization should be a priority if there is any suspicion of occult trauma to the cervical spine. In most emergency rooms, patients who present with an unknown cause of lethargy or loss of consciousness have their blood glucose levels drawn.
The ABCDE approach can be used to assess a critically unwell patient systematically. It involves working through the following steps:
- Airway
- Breathing
- Circulation
- Disability
- Exposure
Each stage of the ABCDE approach involves clinical assessment, investigations, and interventions. Problems are addressed as identified, and the patient is re-assessed regularly to monitor their response to treatment.
Initial treatment of overdose begins with supportive care. This includes assistance in respiration, CPR if no spontaneous circulation is occurring, and removal of the opioid agent if a patch or infusion is delivering it. If the physician suspects that the individual has overdosed on an opioid and has signs of respiratory and CNS depression, no time should be wasted on laboratory studies; instead, naloxone should be administered as soon as possible.
Naloxone is a competitive antagonist of the opiate receptor. It can be administered by intravenous, intramuscular, subcutaneous, or intranasal routes.
Naloxone
Naloxone is a pure competitive antagonist of opiate receptors and has no agonistic activity. This safe drug can be administered intravenously, intramuscular, subcutaneously, or via the endotracheal tube. Recently the FDA approved an intranasal formula showing promise, especially in patients who do not have intravenous access. Whether naloxone is administered via the endotracheal tube or intravenously, the onset of action is within minutes. A second dose can be administered every 2 to 3 minutes. The subcutaneous or intramuscular injection may delay the onset for 3 to 10 minutes. As soon the patient is alert and awake, the dose of naloxone should be disconnected.
Besides naloxone, the 2 new agents on the market to reverse opiate toxicity are nalmefene and naltrexone. Nalmefene has a half-life of 4 to 8 hours, whereas naltrexone has a half-life of 8 to 12 hours. However, the routine use of these longer-acting opiate antagonists is not recommended because of the fear of precipitating a prolonged period of opioid withdrawal.

Starting Dose of Naloxone
The starting dose of naloxone is usually between 0.4 to 1 mg in adults and 0.1 mg/kg in children. In suspected chronic opioid abusers, if the patient is somewhat stable, the naloxone is administered slowly at 0.1 to 0,4 mg IV every 1 to 3 minutes to ensure a more controlled reversal of the opioid effects. If naloxone is administered rapidly in these patients, the patient may also start to feel the pain being suppressed by the opioid.
If the respiration is shallow, the patient can be administered 100% FI02 or assisted with bag-valve ventilation until he or she becomes more alert and cooperative. The onset of action of naloxone is immediate, with a peak response observed within 3 to 8 minutes. A repeat dose may be indicated if the patient still shows signs of opioid toxicity.
It is crucial to start with a low dose of naloxone at a dose of 0.05 to 0.1 mg IV and slowly titrate upwards because the risk of withdrawal symptoms (for example, nausea, vomiting, agitation, pain, and aspiration) are real, especially in patients suspected of having ingested opioids in combination with other CNS depressants like alcohol, tricyclic antidepressants, and benzodiazepines.
In some patients with opioid overdose and long-term drug addicts, peripheral intravenous access can be difficult and in such cases, the naloxone can be administered intramuscularly or intranasally (2 mg). Even with this route, there is a reversal of opioid toxicity within 5 to 10 minutes. The recently available intranasal formula releases 0.4 mg per single dose spray and may have to be repeatedly given.
The half-life of naloxone is about 30 to 45 minutes, with a duration of action between 90 to 180 minutes. The variations exist because of the route of administration and dose. In a patient with no prior opioid use or history of drug abuse, naloxone can be administered via an intravenous infusion without fear of inducing withdrawal symptoms. Still, the patient’s pain may quickly return, and one must have alternative ways to manage the pain. Naloxone infusion is usually administered in D5W or isotonic saline and is necessary to manage overdose caused by long-action opiates like methadone.
In patients who have taken large doses of propoxyphene, methadone, diphenoxylate/atropine, or rainbow fentanyl, much larger doses of naloxone are usually required to reverse the toxicity. Repeat doses of 2 mg may be required every 3 to 4 minutes for 10 mg. If the patient fails to respond to 10 mg of naloxone, the diagnosis of opioid toxicity should be reconsidered.
Many street opioid preparations are adulterated with contaminants, and the response to naloxone is not always complete. If the patient remains in respiratory distress, one must be prepared to intubate the patient. There is a consensus that a steady infusion of naloxone is better than intermittent dosing to treat large overdoses of opioids. While the threat of withdrawal symptoms is real, these symptoms are not life-threatening. A naloxone infusion can be administered at two-thirds of the initial successful dose and over an hour.
While naloxone is very effective if given promptly, its use has long been limited to administration by physicians and paramedics. With the increase in opioid overdoses, there has been a push to allow intranasal medication administration by bystanders. Evidence looking at the efficacy of out-of-hospital naloxone administration is promising. The bioavailability of a concentrated naloxone nasal spray was shown to be about 25%. Fifty percent absorption occurs within 6 to 8 minutes, and maximum blood concentration is achieved at 20 minutes, making this a viable treatment for the community and prehospital use.
Get Help. Get Better. Get Your Life Back.
Searching for Accredited Drug and Alcohol Rehab Centers Near You?
Even if you have failed previously and relapsed, or are in the middle of a difficult crisis, we stand ready to support you. Our trusted behavioral health specialists will not give up on you. When you feel ready or just want someone to speak to about therapy alternatives to change your life call us. Even if we cannot assist you, we will lead you to wherever you can get support. There is no obligation. Call our hotline today.
(844) 597-1011Fentanyl Addiction
Is fentanyl addictive? YES. Some drug dealers mix this lethal narcotic with other drugs, such as heroin, cocaine, methamphetamine, and MDMA. This is because it takes very little to produce a fentanyl high, making it a cheaper option. This is especially risky when people taking drugs don’t realize they might contain synthetic opioids as a cheap but dangerous additive. They might be taking stronger opioids than their bodies are used to and can be more likely to overdose.
Generally, opioid pain relievers are safe when taken briefly and as prescribed by a doctor. However, users abuse them due to the euphoria they produce, in addition to pain relief. As a result, substance abuse happens when you take it in a different way or in a larger quantity than prescribed or without a doctor’s prescription. Substance abuse with this drug can be best medicated in an inpatient program dedicated to opioid addiction treatment.
How long does fentanyl stay in your system? Without awareness, you may become addicted to prescription opioids given to you for a medical condition. Consequently, you will use these drugs intentionally for the high they can provide. The effects on the brain are strong as they can deplete certain chemicals with continued abuse. Classic signs of opioid addiction can be. Eventually, your brain will become dependent on opioids to function normally. Then, you will start needing more opioids just to ward off withdrawal and feel “normal.”
Treatment Options for Fentanyl Addiction
There is a strong link between mental health and substance abuse. Individuals who struggle with mood disorders like depression and anxiety are more susceptible to developing an addiction to drugs or alcohol, often to self-medicate symptoms of their underlying mental health condition. These co-occurring disorders can make each other worse without proper treatment.
To determine the most effective ways to treat opioid addiction, getting an accurate assessment of all the symptoms is crucial. When a mental health professional has evaluated the symptoms, it may be determined that another form of depression is present and needs a particular treatment. Very often, some combination of psychotherapy, medication, and lifestyle changes are effective for coping with functional.
How long does fentanyl stay in your system and overdose? Most patients who have overdosed on opioids and who are reversed with naloxone are admitted for observation for at least 12 to 24 hours. Naloxone has a half-life of one hour, and some long-acting opioids may continue to cause sedation and respiratory depression.
The opiate-overdosed patient is best admitted to a monitored floor. When it comes to a heroin overdose, most patients are admitted because this illicit drug can cause acute lung injury simultaneously. Most patients with acute lung injury usually present early in the course. Patients with heroin overdose who are asymptomatic may not require 24-hour monitoring, but they still need 6 to 12-hour monitoring and discharge as long as the patient’s vital signs remain stable. Others who do require admission need multiple doses or prolonged intravenous infusions of naloxone to reverse the opioid. Admission is prudent if there is any doubt about the patient’s clinical status.
Fentanyl Vaccine Breakthrough
Researchers declare they’ve developed a breakthrough vaccine intercepting fentanyl from entering the brain and eliminating its high effect. The study, published in Pharmaceutics, was led by the University of Houston researchers. The scientists say that the vaccine targets synthetic opioids by blocking their ability to enter the brain. [11]
According to experts, the vaccination had no unfavorable side effects in the lab rats. Clinical studies on people will shortly begin, according to the researchers. Some specialists are holding off on labeling the vaccination a breakthrough just yet, though. The efficacy and safety of this narcotic vaccine in people must be determined, and booster doses may be required. As a result, vaccinated individuals may not have lifetime protection from an overdose. Narcotic vaccination is a promising development in the prevention and treatment of opioid use disorder overall. However, it still has to be thoroughly studied by people and considered for its adoption in the US’s current social and political environment.
How long does fentanyl stay in your system? The higher the drug dose, the longer the drug will stay in your system. The half-life of this drug will also depend on how it was ingested. For example, the half-life of the Fentanyl Citrate Injection is 219 minutes.
Medically-Assisted Detox
Medical detox is often considered the first stage of opioid use disorder treatment. It will help you navigate the complicated withdrawal process but doesn’t address thought and behavior patterns contributing to opioid use. Various treatment approaches and settings can help provide the ongoing support necessary to maintain long-term sobriety after you complete detox.
Cravings are very common during detox and can be challenging to overcome. This often leads to relapse. Constant medical care during residential rehab helps prevent relapse. Clinicians can provide the necessary medication and medical expertise to lessen cravings and the effects of withdrawals.
Patients in withdrawal should be accommodated away from patients who have already completed withdrawal. Healthcare workers should be available 24 hours a day during the opioid withdrawal timeline. Workers should include:
- A doctor who sees patients on admission and is on call to attend to the patient in case of complications;
- Nurses are responsible for monitoring patients in withdrawal, dispensing medications as directed by the doctor, and providing the patient with information about withdrawal.
The withdrawal management area should be quiet and calm. Patients should be allowed to sleep or rest in bed, or to do moderate activities such as walking. Offer patients opportunities to engage in meditation or other calming practices. Patients in withdrawal should not be forced to do physical exercise. There is no evidence that physical exercise is helpful for withdrawal management. Physical exercise may prolong withdrawal and make opioid withdrawal symptoms worse.
Patients in withdrawal may be feeling anxious or scared. Offer accurate, realistic information about drugs and withdrawal symptoms to help alleviate anxiety and fears. Do not try to engage the patient in counseling or other psychological therapy at this stage. A person in withdrawal may be vulnerable and confused; this is not an appropriate time to commence counseling.
During withdrawal, some patients may become disruptive and difficult to manage. There may be many reasons for this sort of behavior. The patient may be scared of being in the closed setting or may not understand why they are in the closed setting. The patient may be disoriented and confused about where they are.
Psychotherapy
Treating opioid addiction and withdrawal requires interprofessional teamwork by psychiatrists, nurses, social workers, therapists, pharmacists, and other healthcare professionals. The patient is initially stabilized in the emergency department before being transferred to inpatient detox. In an inpatient detoxification unit, nurses, therapists, and psychiatrists work together to manage symptoms before a patient is discharged to psychotherapy programs and follow up with a psychiatrist. Several different modalities of psychotherapy have been used in the treatment, including the following:
- Cognitive Behavioral Therapy (CBT) – An effective treatment that involves changing both the patterns of negative thoughts and the behavioral routines which are affecting the daily life of the depressed person for various forms of depression. Cognitive behavior therapy has been evaluated as particularly effective for treating drug addiction and co-occurring disorders.
- Dialectical Behavioral Therapy – A comprehensive mental health and substance abuse treatment program whose ultimate goal is to aid patients in their efforts to build a life worth living. The main goal of DBT is to help a person develop what is referred to as a “clear mind.”
- Person-Centered Therapy – A strategy that allows and encourages clients to understand and resolve their concerns in a safe, supportive environment.
- Solution-Focused Therapy – An approach interested in solutions that can be quickly implemented with a simple first step leading to further positive consequences.
Under federal law 42.CFR 8.12, patients receiving treatment in Opioid Treatment Programs (OTPs) must be able to receive counseling, along with medical, vocational, educational, and other assessment and treatment services. Regardless of what setting medication is provided, it is more effective when counseling and other services are available to provide patients with a whole-person approach and to support their recovery.
Counseling can be done alone or in a group setting and will be utilized before, during, and after treatment. When going through counseling, problems are discussed, and you are taught different tools that aid in helping you to process and to handle your life situations better. Whether alone or in a group, counseling provides comfort and a safe place to be heard and understood. Coupled with an aftercare program, counseling will help you recover successfully.
Dual Diagnosis Treatment
Drug addiction and mental health disorders often co-occur. Traumatic experiences can often result in mental health disorders and substance abuse. Dual-diagnosis rehabilitation treats both of these issues together. The best approach for the treatment of dual diagnosis is an integrated system. This strategy treats both the substance abuse problem and the mental disorder simultaneously. Regardless of which diagnosis (mental health or substance abuse problem) came first, long-term recovery will depend largely on the treatment for both disorders done by the same team or provider.
When the substance is suddenly absent, the body reacts with unpleasant withdrawal symptoms ranging from flu-like to potentially fatal. For this reason, it is advised to taper off opioid use slowly rather than quitting cold turkey and, ideally, with the supervision of a medical professional. Fortunately, several opioid antagonists can help beat opioid addiction at difficult stages. These medications can help mitigate opioid withdrawal effects or intervene if signs of fentanyl overdose or a lethal dose of fentanyl.

Although these dual diagnosis problems often occur together, this does not mean one caused the other, even if one appeared first. It can be hard to figure out which came first. Researchers think that there are three possibilities as to why they occur together:
- Common risk factors may contribute to both mental disorders and substance use disorders. These factors include genetics, stress, and trauma.
- Mental disorders can contribute to drug use and substance use disorders. For instance, people with mental disorders may use drugs or alcohol to try to feel better temporarily. This is known as self-medication. Also, mental disorders may change the brain, making you more likely to become addicted.
- Substance use and addiction can contribute to the development of a mental disorder. Substance use may change the brain in ways that make you more likely to develop a mental disorder.
Naloxone for Fentanyl Overdose
Naloxone is the generic name of a drug (Narcan) that can reverse the effects of an opioid overdose. It works by attaching itself to the same receptors occupied by the harmful opioids and taking their place. By disrupting the link between the harmful opioid and the receptor, Naloxone can immediately reverse the adverse effects of an overdose. This can be life-saving, namely by restoring the ability to breathe.
It is available as an injectable liquid and as a nasal spray. Does narcan work on fentanyl? YES. The most common brand names include Narcan and Evizo. This medication is only effective if administered when an overdose occurs and cannot be used pre-emptively to prevent an opioid overdose.
When To Use Narcan?
Primarily, Narcan is administered in emergency situations consisting of opiate or opioid drug overdose. Intranasal spray is the most common form of Naloxone used in emergency overdose situations outside of medical facility settings. Narcan is also administered intramuscularly (into the muscle), subcutaneously (under the skin), or by intravenous injection.
According to the Substance Abuse and Mental Health Service Administration (SAMHSA), the candidates for naloxone are those who:
- Take high doses of opioids for long-term management of chronic pain
- Receive rotating opioid medication regimens
- Have been discharged from emergency medical care following opioid poisoning or intoxication
- Take certain extended-release or long-acting opioid medication
- Those who have had a period of abstinence include those recently released from incarceration
Narcan is for people who use drugs and other individuals in a position to initiate an early response to evidence of opioid overdose. Eligible Individuals Would Include:
- People who use or are prescribed opioids may have unintended exposure to opioids through other substance use
- Family members, significant others, companions of people who use or are prescribed opioids
- People re-entering the community from correctional settings and their family members
- Early responders to calls for emergency medical assistance (EMTs and paramedics)
- Clinicians and others who provide services to individuals with substance use disorders
- In office-based, clinic, or residential settings
- Corrections staff
- Law enforcement officers
- The team of state and community-based public and private organizations serving
- Populations at high risk for opioid overdose
Buprenorphine
Buprenorphine can activate opioid receptors and relieve cravings without eliciting any surge of euphoria. Thus, being an opioid can fulfill the receptors’ physical need to be stimulated but does so without generating feelings of joy (the leading cause of addiction-forming behavior).
What makes it even more helpful is the limits to the effect this partial opioid can exert on these receptors. This ensures that It can achieve no high, effectively eliminating the likelihood of being abused, and also limits the effects of other opioids that are taken.
This medication functions similarly to methadone, another opioid antagonist commonly used to treat opioid dependence. However, methadone has recently fallen out of favor as a treatment for opioid addiction due to its potential for habit-forming. As such, it has largely been replaced with buprenorphine in opioid addiction treatment settings.
Suboxone
Suboxone is a brand-name drug composed of Naloxone and buprenorphine used to treat opioid dependence, not just manage the symptoms. The buprenorphine component can lessen persisting opioid cravings – the primary side effect of opioid detox or withdrawal. The presence of Naloxone allows Suboxone to take treatment a step further. Instead of reversing the symptoms of an overdose, Naloxone acts as a deterrent to further opioid abuse. It does so by causing unpleasant withdrawal symptoms should Suboxone be used via injection (a typical administration method for drug abusers) instead of being taken orally as directed. This prevents Suboxone users from trading one addiction for another.
When individuals have taken opioids regularly over a sustained period of time (either illicitly or for pain management), physiologic dependence develops, and abrupt cessation of opioids produces a characteristic withdrawal syndrome. Signs and symptoms may include autonomic hyperactivity (sweating, chills, lacrimation, tremor, pupillary dilatation, and piloerection), gastrointestinal distress (nausea, intestinal cramping, diarrhea, vomiting), yawning, rhinorrhea, sneezing, body aches, anxiety, and dysphoria.
Though rarely life-threatening, opioid withdrawal is extremely unpleasant and is a main driver of continued opioid use among those who have developed physiological dependence and/or opioid use disorder. Opioid withdrawal can be treated with a slow taper of opioid dosage – preferably with an agent with a long half-life, such as methadone or buprenorphine – to avoid abrupt variations in systemic exposure to opioids. Opioid withdrawal can also be treated with non-opioid medications such as adrenergic alpha-2 receptor antagonists (e.g. clonidine, lofexidine, guanfacine, tizanidine), which reduce autonomic symptoms, and other symptomatic treatments — e.g. benzodiazepines for anxiety, non-opioid analgesics for pain, or anti-emetics for gastrointestinal distress.
First-class Facilities & Amenities
World-class High-Quality Addiction & Mental Health Rehabilitation Treatment
Rehab Centers TourRenowned Addiction Centers. Serene Private Facilities. Inpatient rehab programs vary.
Addiction Helpline(844) 597-1011Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Success Stories Across Our Network
- Low Patient to Therapist Ratio
- Onsite Medical Detox Center
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Personal Development Events
Fentanyl Test Kit
How long does fentanyl stay in your system, and what about the test strips? Fentanyl test strips are tiny strips of paper that were initially created to detect fentanyl in urine. But you can also use them to see whether a drug includes fentanyl in just a few minutes. How to test for fentanyl? Fentanyl test strips CVS help protect people who use street drugs from overdosing and death fentanyl causes. Learn more about how they work and where to find them. Each strip costs about a dollar. But you might get free strips from your local health department, a needle exchange program, or another community-based organization.
Narcotic test strips aren’t legal everywhere because some states consider them drug paraphernalia (items you need to do drugs). But many health and public policy experts defend their use and other harm-reduction approaches.
In 2021, the CDC and the Substance Abuse and Mental Health Services Administration (SAMHSA) declared that federal grant recipients, such as nonprofit drug treatment and harm-reduction centers, can use grant money to buy these test strips.
Fentanyl Half Life
According to the FDA, fentanyl preserves cardiac stability when medically used and blunts stress-related hormonal changes at higher doses. How long does fentanyl stay in your system, and its half-life? The pharmacokinetics of the narcotic drug can be described as a three-compartment model, with a distribution time of 1.7 minutes, a redistribution of 13 minutes, and a terminal elimination half-life of 219 minutes.
Fast-acting synthetic opioid tablets, lozenges, and nasal sprays take 15 to 30 minutes to work, but they wear off after 4 to 6 hours. The patches can take up to a day or two to start working, but they will last longer. Patches are usually given after tablets.
Medically prescribed fentanyl is typically administered intravenously (IV), intramuscularly (IM), transdermally (TD) as skin patches, intranasally (IN) in the form of a volatile nasal spray, and intrathecally (IT). It is also available as a buccal soluble thin film, which can liquefy in the mouth, similar to the sublingual tablets. Nonetheless, unlike other opioids or opiates, it is less expected to find forms of synthetic drugs such as oral tablets or powders.
A new medication currently being used to address the gastrointestinal (GI) side effects without offsetting its primary analgesic aims acts selectively on the GI mu-opioid receptors and can help in relieving constipation while still providing pain relief, a dilemma previously treated off-label in some hospitals by discontinuing a vial of naloxone in ice water and taking the mix enterally. The transdermal patch is for the long-term management of pain.
Fentanyl comes in an injectable form of 50 mcg/mL. Dosing is as follows by indication:
- Preoperative Analgesia
- 50 to 100 mcg IV/IM for a single dose 30 to 60 minutes before surgery; consider lower dosing in patients 65 and older.
- Anesthesia Adjunct
- 2 to 50 mcg/kg/dose IV for a single dose
- 2 to 20 mcg for low dosing; 20 to 50 mcg for higher dosing. Low dosing is favored in patients 65 and older.
- 2 to 50 mcg/kg/dose IV for a single dose
- Regional Anesthesia Adjunct
- 50 to 100 mcg IV/IM for a single; consider lower dosing in patients 65 and older.
- General Anesthesia
- 20 to 50 mcg/kg/dose IV for a single dose; consider lower dosing in patients 65 and older.
- For high-risk patients undergoing complicated surgical procedures, use oxygen and a muscle relaxant; doses up to 150 mcg/kg/dose may be necessary.
- Post-Operative Pain Control
- 50 to 100 mcg IV/IM every 1 to 2 hours as needed; alternately 0.5 to 1.5 mcg/kg/hour IV as needed. Consider lower dosing in patients 65 and older.
- PCA (patient-controlled analgesia): 10 to 20 mcg IV every 6 to 20 minutes as needed; start at the lowest effective dose for the shortest effective duration – refer to institutional protocols.
- Moderate to Severe Acute Pain (Off-Label)
- 1 to 2 mcg/kg/dose intranasally each hour as needed; the maximum dose is 100 mcg. Use the lowest effective dose for the shortest effective duration.
Fentanyl is a widely used narcotic in the hospital environment. Unfortunately, with current concerns about opioid overdose and toxicity, all interprofessional healthcare team members who prescribe, administer, or dispense this drug should be familiar with its adverse effects and how to reverse them. This includes all clinicians (including mid-level practitioners), nurses, and pharmacists.
When prescribing narcotics, the dose and duration should be the lowest and shortest sufficient, and the patient is continuously evaluated for compliance and/or diversion in treatment settings. Healthcare workers should be aware of new prescribing laws governing opioids, and unlike in the past, observed prescribing of narcotics can lead to legal troubles, including loss of prescription privilege. With interprofessional coordination of activities and open communication, opioid therapy can be successful and adverse events avoided or managed if they arise.

Get Your Life Back
Find Hope & Recovery. Get Safe Comfortable Detox, Addiction Rehab & Dual Diagnosis High-Quality Care.
Hotline(844) 597-1011Carfentanil vs Fentanyl
Carfentanil is a synthetic opioid-related substance not approved for use in humans.
According to the DEA, carfentanil is a synthetic opioid that is 10,000 times more powerful than morphine and 100 times more potent than fentanyl, which is 50 times more potent than heroin. Carfentanil is a Schedule II substance under the Controlled Substances Act and is used as a tranquilizing agent for elephants and other large mammals. The fatal dose range for carfentanil in humans is unknown. However, as noted, carfentanil is roughly 100 times more potent than fentanyl, which can be deadly in the 2-milligram range, depending on the route of administration and other factors.
Carfentanil and other synthetic opioid-related compounds seriously threaten public safety, first responder, medical, treatment, and laboratory personnel. These substances can come in several forms, including powder, blotter paper, tablets, and spray – they can be absorbed through the skin or accidental inhalation by airborne powder. If encountered, responding personnel should do the following based on the specific situation:
Exercise extreme caution. – Only properly trained and outfitted law enforcement professionals should handle any substance suspected to contain the synthetic opioid-related compound. If encountered, contact the appropriate officials within your agency.
Be aware of any sign of exposure. – Symptoms include: respiratory depression or arrest, drowsiness, disorientation, sedation, pinpoint pupils, and clammy skin. The onset of these symptoms usually occurs within minutes of exposure.
Seek IMMEDIATE medical attention. Carfentanil and other synthetic opioid-related substances can work quickly, so it is important to call EMS immediately in suspected exposure. If inhaled, move the victim to fresh air. If ingested and the victim is conscious, wash out the victim’s eyes and mouth with cool water.
Be ready to administer naloxone in the event of exposure. – Naloxone is an antidote for opioid overdose. Immediately administering naloxone can reverse an overdose of carfentanil, or other opioids, although multiple doses of naloxone may be required. Continue administering a dose of naloxone every 2-3 minutes until the individual is breathing on his/her own for at least 15 minutes or until EMS arrives.
Remember that carfentanil can resemble powdered cocaine or heroin. – If you suspect the presence of carfentanil or any synthetic opioid, do not take samples or otherwise disturb the substance, as this could lead to accidental exposure. Rather, secure the substance and follow approved transportation procedures.
Carfentanil drug is one of the newest drugs to take hold in the United States. In recent years, sedative and tranquilizing drugs are accounted for numerous overdose-related deaths because of their high potency both in power and severe effects. Carfentanil was first synthesized in 1974 by a team of chemists. It has since been classified as a Schedule II substance under the Controlled Substances Act. One of the significant risks associated with the drug is that it can come in many forms, including an ingredient paired with another drug. For example, Carfentanil and other synthetic opioids have been found mixed with heroin. This mixture increases the potency of each dosage and makes heroin misuse much more deadly.
According to the World Health Organization, there are currently no controlled laboratory studies involving the abuse potential of Carfentanil in any species, including humans. However, it is classified as a Schedule II drug by the DEA, which means it is a dangerous substance with a high potential for abuse.
Carfentanil addiction is rare. Most drug users don’t purposely abuse Carfentanil alone because it is compelling and deadly. Instead, most drug abusers accidentally ingest the drug while using other recreational substances purchased online from a drug dealer or a friend.
It is difficult for medical experts and organizations to track carfentanil abuse in the U.S. because the drug is so easily hidden in other substances. As a result, many of the resulting overdoses may not even be attributed to Carfentanil, despite its presence.
Fentanyl vs Morphine
Fentanyl is a synthetic opioid up to 50 times stronger than heroin and 100 times stronger than morphine. It is a major contributor to fatal and nonfatal overdoses in the U.S. Morphine is a non-synthetic narcotic (opioid) made from opium, prescribed as Kadian®, MS-Contin®, Oramorph SR®, MSIR®, RMS®, Roxanol®. Very effective for pain relief but high potential for abuse.
FDA-approved usage of morphine sulfate includes mild to severe pain that may be acute or chronic. Most commonly used in pain management, morphine relieves patients tormented with pain. Clinical situations that benefit greatly from medicating with morphine include management of palliative/end-of-life care, active cancer treatment, and vaso-occlusive pain during a sickle cell crisis. Morphine also has off-label uses for painful conditions.
Like any opioid drug, morphine can be lethal when not used appropriately. It causes symptoms related to depression in the central nervous system. Severe respiratory depression is the most feared complication of morphine in cases of overdose. Immediate injection of naloxone is required to reverse the effects of morphine.
Fentanyl vs Heroin
Opioid medications like heroin and synthetic opioids attach to opioid receptors in the brain, decreasing pain perception and enhancing pleasure and relaxation. Both have high potency, act quickly and can be fatal with just one dosage.
Both these opioids are thought to be highly addictive substances. The “high” they may provide is potent and euphoric, and dependency can develop fast. When the body gets dependent on an opioid medicine to operate properly, the brain will develop used to its presence. When the effects of the drugs wear off, severe withdrawal symptoms may appear. These side effects include physical symptoms like the flu and sadness, anxiety, irritability, agitation, and sleeplessness. Taking the drug may seem preferable to dealing with these excruciating withdrawal symptoms, which can soon result in an inability to regulate how much or how frequently the drug is used. Compulsive drug usage brought on by persistent drug use alters brain chemistry.

Regular use of heroin can lead to tolerance. This means users need more and more drugs to have the same effect. At higher doses over time, the body becomes dependent on heroin. If dependent users stop heroin, they have heroin withdrawal symptoms. These symptoms include restlessness, muscle and bone pain, diarrhea and vomiting, and cold flashes with goosebumps.
Heroin is an opioid that binds to receptors in the brain to release the chemical dopamine. But, this release is only temporary, leaving some people wanting more of the “good” feeling. Data from 2011 also showed that an estimated 4 to 6 percent who misuse prescription opioids—a broad group of pain-relieving drugs—switch to heroin. About 80 percent of people who used heroin first misused prescription opioids. [10] Moreover, these prescription opioid pain medicines may include OxyContin® and Vicodin®.
The misuse of prescription opioids sometimes begins with legal drugs like painkillers prescribed after surgery or some other injury. If you become addicted to these prescribed medications and cannot obtain them, you may pursue illegal drugs like opioids to achieve the same pleasurable feeling. Therefore, anyone who takes opioids can be at risk for developing an opioid use disorder or a heroin addiction.
Fentanyl vs Dilaudid
A brand-name drug called Dilaudid contains the morphine-derived semi-synthetic opioid hydromorphone. Dilaudid is used to alleviate symptoms of moderate to severe pain. Dilaudid is often only used for brief therapeutic purposes due to its significant tendency for addiction. Dilaudid is still approximately a tenth as powerful as synthetic opioids, despite being around ten times more potent than morphine. Hydromorphone extended-release tablets relieve severe pain in people who are expected to need pain medication around the clock for a long time and who cannot be treated with other medications.
Hydromorphone extended-release tablets should only be used to treat tolerant people (used to the effects of the medication) to opioid medications because they have taken this type of medication for at least one week and should not be used to treat mild or moderate pain, short-term pain, pain after an operation or medical or dental procedure, or pain that can be controlled by medication that is taken as needed. Hydromorphone is in a class of medications called opiate (narcotic) analgesics. It works by changing how the brain and nervous system respond to pain.
Dilaudid can take up to a half-hour to begin working before it lasts several hours. While a synthetic opioid works faster, sometimes within a minute. However, fentanyl has a relatively short effect and will typically start to wear off within 90 minutes. For this reason, Dilaudid is more often used for long-term pain management, while synthetic opioids are used for immediate effect.
Fentanyl Laced Weed
Several media reports now claim that drug dealers lace cannabis with synthetic opioids. But very little evidence supports this claim. Instead, stories of people overdosing on opioids while using cannabis might be because a person uses opioids while they use cannabis.
Recently, opioid-laced drugs have been uncovered to be circulated in America’s illegal drug trade. Marijuana usage and legalization are both rising in popularity at the same time. While in some of the documented cases, there is a prevalence of synthetic opioid-laced weeds that have been challenging to confirm. That is why it’s best to stick to regulated, legal dispensaries (in states where they’re available). If you’re considering using cannabis products and want further warranties of their safety. There have been intermittent reports of synthetic opioids turning up in marijuana in the U.S.
Synthetic opioids have indeed been confirmed in street drugs, including crack cocaine. The U.S. Drug Enforcement Administration (DEA) notes that opioids’ effects are “intense” and “short-term” and that synthetic opioid is frequently added to heroin as well as other substances.
World-class, Accredited, 5-Star Reviewed, Effective Addiction & Mental Health Programs. Complete Behavioral Health Inpatient Rehab, Detox plus Co-occuring Disorders Therapy.
CALL(844) 597-1011End the Addiction Pain. End the Emotional Rollercoaster. Get Your Life Back. Start Drug, Alcohol & Dual Diagnosis Mental Health Treatment Now. Get Free No-obligation Guidance by Substance Abuse Specialists Who Understand Addiction & Mental Health Recovery & Know How to Help.
Fentanyl Detox
The biggest complication of synthetic opioid withdrawal is returning to drug use. Most deaths from fentanyl occur in people who have just detoxed. The first few days are the most dangerous because those who have just gone through opioid withdrawal can overdose on a much smaller dose than they used. During opioid withdrawal, your tolerance to the drug is reduced. Furthermore, if you stop or cut back on these drugs after heavy use for a few weeks or more, you will have several fentanyl withdrawal symptoms, including:
- Agitation
- Anxiety
- Muscle aches
- Increased tearing
- Insomnia
- Runny nose
- Sweating
- Yawning
- Abdominal cramping
- Diarrhea
- Dilated pupils
- Goosebumps
- Nausea
- Vomiting
How long does fentanyl stay in your system? It can leave your system from 11 to 22 hours. It can appear in urine tests for one to three days after use. Blood testing can detect IV doses for up to 20 hours, oral fentanyl for up to 3 days, and transdermal or patch for up to 3.5 days. Hair testing can detect the use for up to 90 days.
Fentanyl Withdrawal Timeline
How long does fentanyl stay in your system, and its withdrawal effects? Opioid drug withdrawal mostly adheres to a general timeline. In general, the withdrawal symptoms typically peak within 48-72 hours and subside within a period of 5 to 10 days. The onset, duration, and intensity of withdrawal symptoms will be experienced differently by each person.
Early Stage
Generally, mild withdrawal symptoms can be felt as soon as 12 hours after the last dose. However, because this narcotic is slow-acting due to its time-release properties, some people don’t feel any withdrawal symptoms until possibly 20 to 30 hours after the last dose. The early stage usually lasts about two to three days with typical symptoms including:
- Body aches
- Flu-like symptoms (runny nose, sweating, fever, or chills)
- Trouble sleeping
Peak Stage
The peak stage will likely produce the most severe and uncomfortable opioid withdrawal symptoms. This usually appears between days 3 and 5, with common symptoms such as:
- Diarrhea
- Vomiting
- Body aches that extend to the bones
- Continued flu-like symptoms
- Nausea
- Mood swings
- Insomnia
How long does fentanyl stay in your system? Many journals have been released trying to understand the duration of fentanyl in bodily fluids such as urine and saliva. As of the moment, a drug test or drug testing is the surest way to identify “how long does fentanyl stay in your system?.” The duration of how long does fentanyl stay in your system or the time that any drug stays in the body has to do with its elimination half-life. This measures how long the drug takes from its maximum concentration within the blood to half of its maximum concentration.

Late Stage
The severity of withdrawal symptoms ought to be waning after around five days. Physical effects usually go away in a week or two, but psychological problems, like cravings or mood swings, might last for several weeks or months. To avoid a relapse, it is beneficial to have continued professional support throughout this phase.
It is significant to highlight that the danger of overdose is noteworthy if a person relapses while detoxing from any opioid. This is because the body’s tolerance to the drug decreases during the detox process. Relapsed users could take the same dosage they did previously, which is greater than the body can metabolize and results in an overdose. So, to successfully detox from an opioid, it is imperative to seek medical assistance, as this can reduce the risk of recurrence.
How long does fentanyl stay in your system? It can be detected in the body for varying amounts of time depending on the person’s biological makeup, metabolism, and the method of testing used.
According to DSM-5, the following disorders must be ruled out first when treating a patient with opioid withdrawal.
Opioid-Induced Mental Disorders
Commonly co-occurring in opioid drug users and can be characterized by symptoms that occur in primary mental disorders. Such symptoms include depressed mood, persistent depressive disorder (dysthymia), and opioid-induced depressive disorder. Opioid withdrawal differs from other opioid-induced disorders because symptoms in other disorders predominate clinical presentation and warrant further diagnostic investigation.
Other Substance Intoxication
Alcohol intoxication, hypnotic, or anxiolytic intoxication can cause a similar clinical presentation of opioid intoxication and must also be ruled out.
Other Withdrawal Disorders
Sedative-hypnotic withdrawal symptoms may resemble opioid withdrawal characteristics, but opioid withdrawal is also characterized by lacrimation, rhinorrhea, and pupillary dilation. Hallucinogen and stimulant intoxication can also cause pupillary dilation, but other symptoms of opioid withdrawal-like nausea, diarrhea, vomiting, lacrimation, and rhinorrhea, are usually absent.
Fentanyl Rehab
If you are researching now, “How long does fentanyl stay in your system?” instead of asking your doctor, you may think of detoxing at home. Opioid detox at home can be difficult and sometimes unproductive. Unassisted withdrawal may not be life-threatening, but there is a major possibility that it will lead to relapse. When opioid substances such as begin to leave the human blood system, they begin to develop severe cravings for the substance.
Strong cravings and unpleasant flu-like symptoms can make it easy for someone going through withdrawal at home to give up and relapse before their recovery gets in its way. Without the medical and social support, a detox center offers, it is tempting to abandon withdrawal and start using again. Medications and therapy are accessible at a medical detox center to help reduce the discomfort and the risk of relapse compared to detoxing at home.
We Level Up is a trusted treatment center for opioid addiction. Patients in our residential therapy programs at the We Level Up addiction treatment center will live comfortably within the facility during this crucial and fragile time. This supportive environment is designed to give patients 24-hour care for sobriety, removing temptations for relapse and applying an air of recovery into every component of the treatment timeline, including opioid addiction treatment. At We Level Up, we find that clients living in a supportive community, especially during their early recovery process, can truly focus on what matters most: their recovery.
Some of the many modalities applied and practiced within our residential treatment facility are:
- Cognitive Behavioral Therapy
- DBT Therapy
- 12-Step Groups
- Group Therapy
- Alumni Support
- Medically-Assisted Detox
If you’re worried, “How long does fentanyl stay in your system?” Medical opioid detox helps smooth withdrawal, reduces side effects, prevents serious complications, and lessens opioid cravings. Professional treatment offers a decent start toward recovery and helps maintain long-term sobriety. Opioid detox has to be followed with counseling, education and awareness, family and individual therapy, and support groups that can aid an individual in their attempt to stop using drugs and continue sobriety.
Above all, we’re passionate about providing the best care and treatment options for clients and their families. Our treatment team is dedicated to giving each and every client the best chance for recovery. Finding a trusted addiction and mental health rehabilitation center is critical to finding the best treatment options.
A great way to weed through to uncover the best recovery programs should include seeking accredited organizations like We Level Up. If you or a loved one is struggling with opioid addiction, you may contact us. Our counselors are always ready to answer any possible questions, such as “How long does fentanyl stay in your system? Your call is private and confidential.
Top 10 Fentanyl Drug FAQs
-
What is fentanyl used for?
Pharmaceutical fentanyl dose is a synthetic opioid approved for treating severe pain, typically advanced cancer pain.
-
How long does fentanyl stay in your system?
A person can test positive for fentanyl exposure on a urine test for 24–72 hours after the last use. However, Norfentanyl, a metabolite created while breaking down the drug in the body, can be detected in a fentanyl drug test for up to 96 hours. Hair tests can detect how long does fentanyl stay in your system and its metabolites for up to 3 months after the last use.
-
How is fentanyl made?
Fentanyl powder or pills are synthetic opioids originally developed as analgesic or painkiller for surgery. It has a specific chemical structure with multiple areas that can be modified, often illicitly, to form related compounds with marked discrepancies in potency.
-
What does fentanyl do to you?
Like other opioid analgesics, fentanyl effects include relaxation, euphoria, pain relief, sedation, confusion, drowsiness, dizziness, nausea and vomiting, urinary retention, pupillary constriction, and respiratory depression.
-
Where does fentanyl come from?
Who makes fentanyl? and where is fentanyl made? Most fentanyl pills candy, powdered fentanyl, and China fentanyl are mass-produced in Mexico using chemicals from China before being pressed into pills or mixed with other counterfeit pills made to look like Xanax, Adderall, or oxycodone. The counterfeit drugs are then sold to unaware buyers. This is according to the DEA.
-
Is fentanyl an opiate?
It is a synthetic opioid, not an opiate. Together with other drugs, it is used for anesthesia.
-
How long does fentanyl stay in urine?
One study showed that in patients with OUD and chronic fentanyl overdose signs, urinary fentanyl dosage and metabolites could be detected 2–3 weeks after last use when hospitalized in a treatment program.
-
What is fentanyl made from?
As a synthetic opioid, powder fentanyl is not made from poppy but chemicals sourced from large industrial chemical sectors in China and India.
-
Why is fentanyl so dangerous?
Fentanyl patch doses and illegal fentanyl skittles (fentanyl in candy packaging) are synthetic opioids up to 50 times stronger than heroin and 100 times stronger than morphine. It is a major contributor to fatal and nonfatal drug overdoses.
-
How much fentanyl can kill you?
Drug rainbow fentanyl is a deadly drug found in illicit street drugs. Addicts who buy fentanyl lethal doses illegally or on the street frequently misuse it. According to test findings, 2 out of every 5 confiscated fake pills have deadly levels, which the DEA classifies as 2 mg of fentanyl structure. However, because lab-produced fentanyl dosing and its analogs come in so many variations and are frequently mixed with other illegal substances, it is exceedingly challenging to pinpoint the exact dosage that would cause death.
What Does Fentanyl Taste Like?
Rainbow fentanyl may be found in pills, powder, and heroin. You can’t smell or taste rainbow fentanyl. It is a synthetic opioid that has no taste. Fentanyl is odorless and is usually administered as a patch, injection, or lozenge to treat pain. It is a powerful opioid pain medication, producing effects much greater than other commonly prescribed drugs like morphine and oxycodone. Because of its potency, it should only be taken under medical supervision to reduce the risk of overdose. Long-term use of opioids can lead to tolerance and dependence, which may require medical treatment to prevent adverse side effects and withdrawal symptoms.
Fentanyl and Alcohol
Some substances, like alcohol, have both stimulant and depressant effects. Alcohol may have initial effects that mimic those of stimulants. However, it mainly slows the body down, making it a depressant. Alcohol slows the heart rate and breathing and dulls reflexes and response time through interactions with the central nervous system (CNS). In other words, it depresses multiple systems in the body that rely on communication with the CNS to function correctly. As a result, alcohol can cause slurred speech, disturbed perceptions, distorted judgment, lessening inhibitions, and an inability to react quickly.
Alcohol can make a medication less effective or even useless, harmful or toxic to your body. Some medicines that you might never have suspected can react with alcohol, including many medications which can be purchased “over-the-counter”—that is, without a prescription. Even some herbal remedies can have harmful effects when combined with alcohol. As alcohol exacerbates the effects of opioids, taking fentanyl and drinking alcohol heightens your risk of severe mental and bodily damage and can cause you to overdose unintentionally. Taking them together can cause irregular heart rate, respiratory arrest, coma, and even death.
Effects of Fentanyl Abuse
Rainbow fentanyl affects chemicals in the brain and can cause significant impairment to the mental health of those who abuse it. In addition to these effects on mental health, addiction to this drug has a unique effect on memory and cognition that has not been seen in other opioid abuse and addiction patients. Addiction to opioids may also increase the likelihood of a person engaging in risky behaviors over time. These behaviors may result in physical harm from fights, sexual trauma, or diseases associated with exposure to bodily fluids. In addition to the overall effects of opioid abuse on the body, some unwanted effects are attributed to the method used to ingest opioids, like injecting, snorting, and smoking.
Fentanyl Abuse Signs
Rainbow fentanyl abuse signs and symptoms may be similar to abuse and addiction symptoms to other opioid-related drugs. However, if a person has a prescription for this narcotic and they become addicted, they may frequently “lose” their prescription as a way to get more drugs. Doctor shopping may also be an issue with prescription opioid addiction. People addicted to prescription drugs may even steal family and friends’ prescriptions to get high. There are physical, emotional, and behavioral signs and symptoms of addiction that people need to consider.
The abuse of and dependence on prescription painkillers has reached epidemic proportions in the United States and worldwide. According to federal U.S. data, an estimated 2.1 million people in the United States suffered from substance use disorders related to prescription opioid pain relievers in 2012. According to the U.S. Centers for Disease Control and Statistics, 78 Americans die daily from opioid-related overdose, including prescription medications and illicit opioids.
Addiction Recovery Story of Alcoholism, Opiates Drugs Abuse Video
Joey’s Addiction Recovery Testimonial.
Joey talks candidly on video about his Opiates drugs abuse treatment success and his personal road to recovery.
“My name’s Joey. I have almost two years clean and sober from opiates, alcohol, recreational drugs; you name it.
Something that hit me hard was the death of my firstborn son, Joe, who was twenty-six years old and died of fentanyl. You know, it’s something that I have to carry every day, and you know, when I heard that news, it was right before last Christmas.
The first thing I wanted to do was pick up a bottle, but you know, just through the rooms of NA, AA, you know, having people in the program to lean on and support me. I was able not to pick up that drink or drug and stay clean and sober.
With that, you know, I’m proud of the fact that I went to treatment, and you know, it turned my life around. And I know that you can, you know, live happily and freely without the use of drugs and alcohol.
You know, you will totally live a different life.”
Does Fentanyl Addiction Treatment Work?
Nine months after being discharged, 85% and 95% of those who successfully finish drug rehab report abstaining from all substances. After finishing drug and alcohol rehab, around 80% of patients say their quality of life and health have improved.
Experience Transformative Recovery at We Level Up Treatment Centers.
See our authentic success stories. Get inspired. Get the help you deserve.
Start a New Life
Begin with a free call to an addiction & behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up Treatment Center Network delivers recovery programs that vary by each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- World-class Amenities
- Licensed & Accredited
- Renowned w/ 100s 5-Star Reviews
We’ll Call You
Search We Level Up Fentanyl Detox, Mental Health Topics & Resources
Sources
[1] Factsheets – (DEA) Drug Enforcement Administration
[2] Drug Epidemic – U.S. Department of Health and Human Services National Institutes of Health
[3-4] Fentanyl Facts – (CDC) Centers for Disease Control and Prevention
[5] Fentanyl Awareness – (DEA) Drug Enforcement Administration, With the topic: “Fentanyl Overdose Symptoms”
[6] Accidental Exposures to Fentanyl Patches Continue to Be Deadly to Children – (FDA) U.S. Food & Drug Administration
[7] Fentanyl Patch – U.S. Department of Health and Human Services National Institutes of Health. About the topic: “Fentanyl Patch Overdose Symptoms”
[8] Lifesaving Naloxone – (CDC) Centers for Disease Control and Prevention
[9] Ramos-Matos CF, Bistas KG, Lopez-Ojeda W. [Updated 2022 May 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459275/
[10] Taylor KP, Singh K, Goyal A. Fentanyl Transdermal. [Updated 2022 Nov 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555968/
[11] Haile CN, Baker MD, Sanchez SA, Lopez Arteaga CA, Duddupudi AL, Cuny GD, Norton EB, Kosten TR, Kosten TA. An Immunconjugate Vaccine Alters Distribution and Reduces the Antinociceptive, Behavioral, and Physiological Effects of Fentanyl in Male and Female Rats. Pharmaceutics. 2022; 14(11):2290. https://doi.org/10.3390/pharmaceutics14112290