What are Opioid Withdrawal Symptoms?
Abuse of heroin and prescription opioids is a long-time concern in the US. The chemical makeup of an opioid such as heroin is the same as that of pain relievers, and both can be very addictive and cause deadly opioid overdoses.
People dependent on opioids can experience unpleasant and uncomfortable withdrawal symptoms when they stop using them. Many people describe it as having bad flu, fever and sweating, nausea and vomiting, muscle aches and pain, and insomnia. Unfortunately, some individuals who abuse prescription opioids may turn to heroin as a cheaper and more readily available alternative.
Heroin belongs to the same class of drugs as opioids and can produce similar effects. The transition from prescription opioids to heroin is often driven by increasing tolerance, difficulty accessing prescription medications, or seeking a more potent high. It is crucial to address opioid withdrawal symptoms and addiction promptly to prevent the progression to more hazardous substances like heroin and seek appropriate support.
Symptoms of Opioid Withdrawal
What are the symptoms of opioid withdrawal? For many people, withdrawal is the most challenging barrier to recovery because all its unpleasant symptoms make sufferers believe the only way to stop the pain is to use it again. Therefore, understanding the fundamentals of opioid withdrawal is crucial in preparing for treatment and long-term recovery.
Here is a list of common symptoms that can occur during opioid withdrawal:
- Restlessness and irritability.
- Anxiety and agitation.
- Insomnia and sleep disturbances.
- Muscle aches and pain.
- Excessive sweating.
- Chills and goosebumps (piloerection).
- Runny nose and teary eyes.
- Dilated pupils.
- Yawning.
- Abdominal cramps.
- Nausea and vomiting.
- Diarrhea.
- Increased heart rate and blood pressure.
- Fatigue and weakness.
- Tremors or shaking.
- Difficulty concentrating or “foggy” thinking.
- Drug cravings and a strong desire to use opioids.
Opioid Withdrawal Timeline
Opioid withdrawal symptoms and timeline depend on the specific opioid used, the duration and dosage of use, and individual differences. However, here is a general timeline that represents the progression of opioid withdrawal symptoms:
| Stages of Symptoms | Duration |
| Early symptoms | Early symptoms may emerge within 6-12 hours after the last use. These can include anxiety, restlessness, drug cravings, muscle aches, and insomnia. |
| Peak symptoms | Within 1-3 days, opioid withdrawal symptoms typically reach their peak intensity. During this time, individuals may experience more observable symptoms such as abdominal cramps, nausea, vomiting, diarrhea, dilated pupils, sweating, chills, and increased heart rate. |
| Subsiding symptoms | After about 5-7 days, the acute phase of withdrawal tends to subside, and symptoms gradually diminish. |
Skip To:
Learn More:
- Opiate Withdrawal Symptoms, Can You Die From Opiate Withdrawal?
- How Long Do Opiates Stay in Your System, Body, Blood, and Urine?
- Opioid Withdrawal Timeline
- Opiate Withdrawal Restlessness
- Oxycodone Withdrawal Symptoms, Timeline & Treatment
- Heroin Detox Timeline, Withdrawal Symptoms, Care & Treatment
- Fentanyl Detox Timeline, Withdrawal Symptoms & Treatment
- Percocet Withdrawal Symptoms, Timeline, Effects, Detox Tappering Dangers
- Opioid Crisis
- Opioid Addiction Treatment
Causes of Opioid Withdrawals
The primary cause of opioid withdrawal is the body’s dependence on opioids due to prolonged exposure.
Some common causes of opioid withdrawals include:
- Tolerance: Prolonged use of opioids can lead to tolerance, where higher doses are required to achieve the same effects.
- Physical dependence: With regular opioid use, the body becomes physically dependent on opioids to function properly.
- Medication cessation: If a person has been prescribed opioids for medical reasons, such as managing pain, and the medication is discontinued or reduced, withdrawal symptoms may occur.
- Illicit opioid use: Individuals who use opioids illicitly, such as heroin or illegally obtained prescription opioids, may experience withdrawal symptoms when they run out of supply and attempt to quit.
When opioids are consistently present, the body adapts to their presence and becomes reliant on them to function normally. When opioid use is abruptly stopped or reduced, the body reacts to the absence of opioids, leading to withdrawal symptoms.
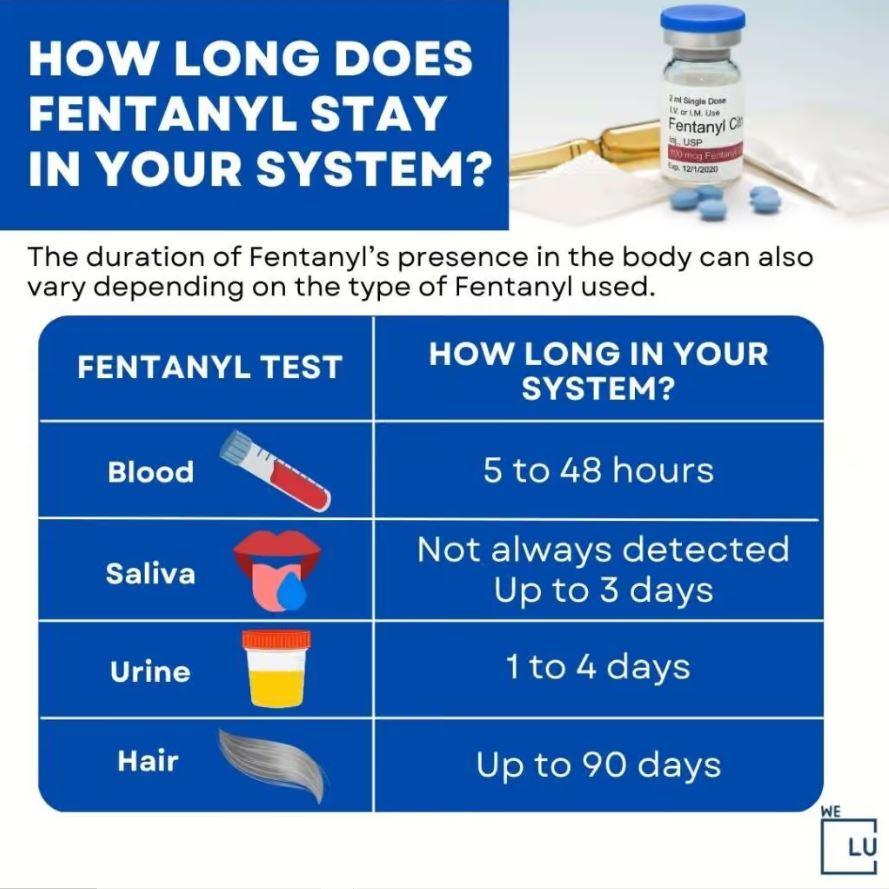
How Long Does Fentanyl Stay In Your System? Infographic
Fentanyl is another potent synthetic opioid significantly more powerful than many other opioids, including heroin and morphine. It is used medically for severe pain management and illegally produced and sold on the illicit drug market. Due to its potency, fentanyl can cause severe physical dependence and addiction, leading to opioid withdrawal symptoms when its use is discontinued or reduced.
Withdrawal from fentanyl can be particularly challenging and intense. The opioid withdrawal symptoms associated with fentanyl are similar to those of other opioids but can be more severe. These symptoms may include:
- Intense drug cravings.
- Restlessness and agitation.
- Severe anxiety and panic attacks.
- Muscle aches and pains.
- Nausea, vomiting, and diarrhea.
- Insomnia and sleep disturbances.
- Sweating and chills.
- Elevated heart rate and blood pressure.
- Tremors and shaking.
- Depression and mood swings.
Embed the below “How Long Does Fentanyl Stay In Your System?” Infographic to your Website. This fentanyl drug infographic is provided by the We Level Up addiction treatment center team. To use the above infographics, you agree to link back and attribute its source and owner at https://welevelup.com/addiction/opioid-withdrawal-symptoms/
How Long Does Fentanyl Stay In Your System? Infographic image link: https://welevelup.com/wp-content/uploads/2023/06/How-Long-Does-Fentanyl-Stays-In-Your-System.jpg
Opioid Withdrawal Protocol Fact Sheet
Inpatient Rehab for Opioid Withdrawal Symptom Management
Inpatient rehab treatment for opioid withdrawal typically involves a structured and supervised protocol designed to manage withdrawal symptoms and support the individual through safe detoxification.
Here is a general outline of the opioid withdrawal protocol in an inpatient rehab treatment:
Assessment
Upon admission, the individual undergoes a comprehensive assessment by medical professionals to evaluate their overall health, level of opioid dependence, medical history, and any co-occurring mental health conditions. Professionals often use clinical opioid withdrawal scales or opioid withdrawal score systems to assess the severity of withdrawal symptoms and guide treatment decisions.
Medical Stabilization
Medical interventions may be used to stabilize the individual’s condition if necessary. This may include administering medications to alleviate opioid withdrawal symptoms and manage potential complications.
Medication-Assisted Treatment (MAT)
Medication-assisted treatment may be provided based on the individual’s needs and the rehab center’s approach. Medications such as buprenorphine, methadone, or naltrexone may help ease opioid withdrawal symptoms, reduce cravings, and support recovery.
24/7 Supervision and Support
Inpatient rehab provides round-the-clock medical supervision and support from trained professionals who monitor the individual’s progress, manage symptoms, and ensure their safety throughout withdrawal.
Emotional Support and Counseling
In addition to medical care, inpatient rehab programs offer counseling, therapy, and support groups to address addiction’s psychological and emotional aspects. This may involve individual therapy sessions, group therapy, or specialized therapies such as cognitive-behavioral therapy (CBT) or motivational interviewing.
Individualized Treatment Plan
A personalized treatment plan is developed based on the individual’s needs and goals. This plan may include ongoing therapy, relapse prevention strategies, and aftercare planning to support the individual’s long-term recovery.
As the individual progresses through the withdrawal process and their condition stabilizes, they may transition from the intensive withdrawal management phase to other components of the rehab program, such as therapy, education, and skill-building activities.
Tapering Opioids For Chronic Pain by CDC
Tapering down prescription opioids is crucial to minimizing or avoiding opioid withdrawal symptoms when discontinuing. Tapering involves gradually reducing the dosage of opioids over a specific period, allowing the body to adjust to lower levels of the drug. This approach helps mitigate the severity of opioid withdrawal symptoms and provides a smoother transition to abstinence.
Download the free file below and have a copy of a pocket guide to tapering opioids for chronic pain. This free pdf has been publicly available for download by the CDC (Centers for Disease Control and Prevention.)

Get Your Life Back
Find Hope & Recovery. Get Safe Comfortable Detox, Addiction Rehab & Dual Diagnosis High-Quality Care.
Hotline(844) 597-1011Opioid Epidemic Statistics
The opioid epidemic has profoundly impacted communities across the United States, straining healthcare systems, law enforcement, and social services. It has resulted in high economic costs, increased rates of infectious diseases such as hepatitis C and HIV, and a growing number of children entering the foster care system due to parental opioid use disorders.
9.7 Million
In 2019, an estimated 9.7 million people aged 12 or older in the US misused prescription opioids in the past year.
Source: CDC
745,000
In 2019, an estimated 745,000 people aged 12 or older in the US reported using heroin in the past year.
Source: CDC
70,630
In 2019, there were roughly 70,630 drug overdose deaths in the US. Opioids were involved in nearly 50,000 deaths, accounting for approximately 70% of all drug overdose deaths.
Source: CDC
Diagnosing Withdrawal Symptoms of Opioid Dependence
Diagnosing withdrawal symptoms of opioid dependence is typically done through medical assessment and clinical evaluation. Healthcare professionals, such as doctors or addiction specialists, use their expertise and standardized diagnostic criteria to evaluate an individual’s symptoms and determine if they are consistent with opioid withdrawal.
Here’s an overview of the diagnostic process:
Medical Assessment: A comprehensive medical assessment is conducted to gather information about the individual’s opioid use history, including:
- The type of opioids used.
- Duration and frequency of use.
- Any previous attempts to quit or reduce opioid use.
- Symptom Evaluation: The healthcare professional will evaluate the individual’s symptoms to determine if they meet the criteria for opioid withdrawal. The presence and severity of opioid withdrawal symptoms, as well as their temporal relationship to opioid cessation or reduction, are crucial considerations.
- Diagnostic Criteria: The healthcare professional will refer to established diagnostic criteria, such as those outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), to determine if the individual’s symptoms meet the criteria for a diagnosis of opioid withdrawal. The DSM-5 criteria include specific symptom criteria, the temporal relationship to opioid use, and the impairment or distress caused by the symptoms.
- Differential Diagnosis: The healthcare professional will also consider other potential causes of the individual’s symptoms to rule out alternative explanations. This may involve assessing for other medical conditions, mental health disorders, or substance use disorders other than opioids that could contribute to the presenting symptoms.
Diagnosing opioid withdrawal is typically part of a broader assessment of opioid use disorder or substance use disorder. A comprehensive evaluation should consider withdrawal symptoms and other aspects, such as impaired control over opioid use, social and occupational impairment, and continued use despite negative consequences.
Get Help. Get Better. Get Your Life Back.
Searching for Accredited Drug and Alcohol Rehab Centers Near You?
Even if you have failed previously and relapsed, or are in the middle of a difficult crisis, we stand ready to support you. Our trusted behavioral health specialists will not give up on you. When you feel ready or just want someone to speak to about therapy alternatives to change your life call us. Even if we cannot assist you, we will lead you to wherever you can get support. There is no obligation. Call our hotline today.
(844) 597-1011How Long Do Opioid Withdrawal Symptoms Last?
The symptoms opioid withdrawal timeline depends on the type of opioid you are taking. Longer-acting opioids like fentanyl and methadone take longer to leave the body, so withdrawal symptoms usually don’t emerge until 12 to 48 hours after the last use. Withdrawal from these opioids also lasts anywhere from 10 to 20 days.
For short-acting opioids like heroin or oxycodone, withdrawal may last 3 to 5 days. Ways to treat mild opioid withdrawal include increased water and vitamin intake, while more severe withdrawal may require opioid use disorder medication and opioid detox treatment.
Opioid Withdrawal Complications
Opioid withdrawal symptoms aren’t typically life-threatening. But the effects of other health conditions can lead to severe problems. For example, a higher pulse or blood pressure can cause issues if you have a heart condition.
Other complications of opioid withdrawal symptoms include:
- Vomiting and diarrhea lead to dehydration, high blood sodium levels (hypernatremia), and heart failure.
- Leaking or bleeding amniotic fluid in pregnant women.
- Higher risk of an opioid overdose because your tolerance is lower. If you start using the opioid again, you’ll need a smaller dose than usual.
- Intense psychological symptoms, including anxiety, depression, and mood swings, often accompany opioid withdrawal symptoms. These emotional disturbances can be challenging to cope with and may increase the risk of self-harm or relapse.
The discomfort and cravings experienced during withdrawal can increase the likelihood of relapse. Suppose a person relapses and returns to opioid use after a withdrawal period. In that case, their tolerance may be reduced, putting them at higher risk of accidental overdose due to taking the same dose they previously used.
First-class Facilities & Amenities
World-class High-Quality Addiction & Mental Health Rehabilitation Treatment
Rehab Centers TourRenowned Addiction Centers. Serene Private Facilities. Inpatient rehab programs vary.
Addiction Helpline(844) 597-1011Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Success Stories Across Our Network
- Low Patient to Therapist Ratio
- Onsite Medical Detox Center
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Personal Development Events
Opioid Withdrawal Treatment
Opioid withdrawal treatment involves various approaches to managing withdrawal symptoms, supporting individuals through detoxification, and facilitating long-term recovery. Here are some common treatment options for opioid withdrawal:
- Medication-Assisted Treatment (MAT): MAT involves using medications for opioid withdrawal approved by the FDA to help reduce withdrawal symptoms, alleviate cravings, and support recovery. Medications commonly used in MAT include methadone, buprenorphine, and naltrexone.
- Medical Detoxification: Medical detoxification involves supervised withdrawal in a controlled environment, typically in an inpatient or outpatient setting. Addiction treatment professionals monitor the individual’s vital signs, manage opioid withdrawal symptoms, and provide medical interventions to ensure their safety and comfort during withdrawal.
- Behavioral Therapies: Various behavioral therapies address the psychological and emotional aspects of opioid dependence and withdrawal. These therapies aim to modify patterns of thinking and behavior related to drug use, develop coping skills, and prevent relapse. Examples include cognitive-behavioral therapy (CBT), contingency management, and motivational interviewing.

- Supportive Care: Providing a supportive and compassionate environment is essential during opioid withdrawal treatment. This may involve emotional support, counseling, peer support groups, and education about addiction and recovery. Supportive care helps individuals navigate withdrawal challenges and build a foundation for long-term recovery.
- Aftercare Planning: After completing the initial withdrawal phase, individuals benefit from developing an aftercare plan to support their ongoing recovery. This may include continued therapy, participation in support groups, and access to resources for maintaining sobriety and addressing any underlying issues contributing to opioid use.
- Evidence-Based Approaches: Complementary and holistic therapies, such as mindfulness techniques, acupuncture, yoga, and exercise, can be integrated into opioid withdrawal treatment. These holistic activities promote overall well-being, stress reduction, and self-care, enhancing recovery.
Treatment for opioid withdrawal should be individualized, and the treatment approach may depend on factors such as the severity of opioid dependence, individual preferences, and available resources. Seeking professional help from healthcare providers, addiction specialists, or substance abuse treatment centers is crucial for comprehensive assessment and appropriate treatment planning.
Opioid Withdrawal Medications
There are several medications used in the management of opioid withdrawal symptoms. These medications primarily aim to reduce the severity of withdrawal symptoms, alleviate cravings, and support recovery. Here are some common medications used for opioid withdrawal:
- Methadone: Methadone is a long-acting opioid agonist that helps stabilize individuals with opioid dependence. It can be used for both detoxification and maintenance treatment. Methadone reduces opioid withdrawal symptoms and cravings while minimizing the risk of severe withdrawal. It is typically dispensed through specialized clinics.
- Buprenorphine: Buprenorphine is a partial opioid agonist that activates opioid receptors more mildly than full opioid agonists like heroin or oxycodone. It can be used for detoxification or as a maintenance treatment. Buprenorphine reduces opioid withdrawal symptoms and cravings while lowering the risk of respiratory depression and overdose.
- Naltrexone: Naltrexone is an opioid receptor antagonist that blocks the effects of opioids. It is primarily used for relapse prevention once detoxification has been completed. Naltrexone helps reduce cravings and can be administered orally or as a monthly injectable (Vivitrol).
- Clonidine opioid withdrawal medication: Clonidine is not an opioid, but it is commonly used off-label to manage certain symptoms of opioid withdrawal. Clonidine is most effective for which symptom of opioid withdrawal aggravate anxiety, agitation, sweating, and elevated blood pressure. Clonidine for opioid withdrawal can help alleviate some of the autonomic symptoms associated with withdrawal.
- Symptom-specific medications: Other medications may be used to manage specific symptoms of opioid withdrawal. For example, over-the-counter or prescription medications can be used to address gastrointestinal symptoms (e.g., loperamide for diarrhea), sleep disturbances (e.g., sedating antihistamines), or muscle aches (e.g., nonsteroidal anti-inflammatory drugs).
The choice of medication and treatment approach depends on factors such as the individual’s specific needs, the severity of opioid dependence, medical history, and treatment goals.
If you don’t know where to start or looking into different options to treat opioid withdrawal symptoms, connect with We Level Up treatment center. We can help you explore different programs based on your unique case. Call us today to get started. Each call is private and confidential.
World-class, Accredited, 5-Star Reviewed, Effective Addiction & Mental Health Programs. Complete Behavioral Health Inpatient Rehab, Detox plus Co-occuring Disorders Therapy.
CALL(844) 597-1011End the Addiction Pain. End the Emotional Rollercoaster. Get Your Life Back. Start Drug, Alcohol & Dual Diagnosis Mental Health Treatment Now. Get Free No-obligation Guidance by Substance Abuse Specialists Who Understand Addiction & Mental Health Recovery & Know How to Help.
Top 5 Opioid Withdraw Symptoms FAQs
-
How long does opioid withdrawal last?
The duration of opioid withdrawal is determined by several factors, including the specific opioid used, the duration and dosage of use, and individual differences. Generally, the acute phase of withdrawal, characterized by intense symptoms, lasts about 5-7 days. However, some individuals may experience lingering mild symptoms for weeks or months after the acute phase has resolved.
-
Can you die from opioid withdrawal?
The opioid withdrawal itself is not considered life-threatening. However, in rare cases, complications associated with severe dehydration, electrolyte imbalances, or other underlying medical conditions may occur during withdrawal and risk an individual’s health. It is crucial to seek medical assistance and support from healthcare professionals during withdrawal to manage any potential complications effectively.
-
How to get opioid withdrawal meds?
Obtaining medication for opioid withdrawal typically requires a medical evaluation and prescription from a healthcare professional. To get opioid withdrawal medication, seeking help from healthcare providers such as doctors, addiction specialists, or detoxification programs is recommended. They can assess your situation, determine the appropriate medication for your specific needs, and guide you through obtaining and safely using withdrawal medications.
-
Is it effective to take gabapentin for opioid withdrawal?
Gabapentin has been used off-label to manage certain symptoms of opioid withdrawal, such as anxiety, insomnia, and restlessness. While some evidence supports its effectiveness in reducing withdrawal symptoms, more research is needed to fully establish its role and optimal dosing in treating opioid withdrawal. It is important to consult with a healthcare professional who can assess your situation and determine the most appropriate treatment plan.
-
Can I use Kratom for opioid withdrawal?
Kratom, a plant native to Southeast Asia, has been promoted as a natural remedy for opioid withdrawal. While some individuals report anecdotal benefits, the scientific evidence on its effectiveness and safety for opioid withdrawal is limited and conflicting. It is crucial to consult with a healthcare professional before using kratom for opioid withdrawal, as it can have potential risks and interactions with other medications.
How Long Do Opiates Stay in Your System? How Long Do Opiates Stay in Urine, Blood, & Body?
Opiates and opioids are drugs derived from opium or synthetic compounds that mimic the effects of opium. Opiates specifically refer to natural substances derived from the opium poppy, such as morphine and codeine. On the other hand, opioids encompass a broader category that includes both natural opiates and synthetic or semi-synthetic drugs, such as oxycodone, hydrocodone, and fentanyl.
Withdrawal refers to symptoms that occur when a person stops or reduces their use of opioids after prolonged and regular use. Opioid withdrawal can be an uncomfortable and distressing experience, but it is not life-threatening. The severity and duration of withdrawal symptoms can vary based on several factors, including the specific opioid used, the duration and dosage of use, and individual differences.
If you’re entering a detox program or worried about an upcoming job drug test, you might want to know how long opiates stay in your system. Watch the video below to learn more.
If you or a loved one is struggling with opioids or opiates addiction, or other substance use disorder(s), call for a FREE consultation 24/7 at (561) 678-0917
Get FREE addiction treatment insurance check – https://welevelup.com/rehab-insurance/
How Long Do Opiates Stay in Your System? Video Transcript
Drugs in the opioid class are used to treat pain. Natural opioids, semi-synthetic opioids generated from natural opioids, and synthetic opioids produced in a lab are all referred to as opioids under the general term. A class of medications known as opioids contain opiates, which are organic byproducts of the poppy plant. The main difference is that “opiate” refers to the substances derived from the opium (poppy) plant. At the same time, “opioids” are all substances that interact with opioid receptors, including those created in the lab.
The length of time that opiates remain in your system varies depending on the type of opiate, the dosage, and the frequency of use. Generally, opiates can stay in your system for two to four days. However, heavier and chronic users may have residues in their system for up to seven days.
Opiates can be detected in the blood test for up to 24 hours and the urine test for up to three days. Opiates can be detected in the hair follicles for up to 90 days. In chronic users, opiates can stay in the body for up to 30 days.
Opiates often have short half-lives, meaning their effects can linger for several hours even though they swiftly leave the body. However, Opioids can linger in a person’s bloodstream for several hours or days after the symptoms subside, depending on the substance used. Urine tests, one of the more common types of drug testing, can identify opioid usage for longer periods, often up to three to four days, and some tests can identify opioid use for up to three months.
Experience Transformative Recovery at We Level Up Treatment Centers.
See our authentic success stories. Get inspired. Get the help you deserve.
Start a New Life
Begin with a free call to an addiction & behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up Treatment Center Network delivers recovery programs that vary by each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- World-class Amenities
- Licensed & Accredited
- Renowned w/ 100s 5-Star Reviews
We’ll Call You
Search We Level Up Opioid Withdrawal Symptoms Detox, Mental Health Topics & Resources
Sources:
[1] Dydyk AM, Jain NK, Gupta M. Opioid Use Disorder. [Updated 2022 Jun 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553166/
[2] Azadfard M, Huecker MR, Leaming JM. Opioid Addiction. [Updated 2023 Jan 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448203/
[3] Clinical Guidelines for Withdrawal Management and Treatment of Drug Dependence in Closed Settings. Geneva: World Health Organization; 2009. 4, Withdrawal Management. Available from: https://www.ncbi.nlm.nih.gov/books/NBK310652/
[4] Institute of Medicine (US) Committee on Opportunities in Drug Abuse Research. Pathways of Addiction: Opportunities in Drug Abuse Research. Washington (DC): National Academies Press (US); 1996. B, Drug Abuse Research in Historical Perspective. Available from: https://www.ncbi.nlm.nih.gov/books/NBK232965/
[5] Opiate and opioid withdrawal – U.S. Department of Health and Human Services National Institutes of Health Available from: https://medlineplus.gov/ency/article/000949.htm
[6] Prescription Opioids DrugFacts – National Institute on Drug Abuse (NIDA)
[7] Understanding the Opioid Overdose Epidemic – Centers for Disease Control and Prevention (CDC)
[8] Schiller EY, Goyal A, Mechanic OJ. Opioid Overdose. [Updated 2022 Sep 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470415/
[9] Narcotics (Opioids) – Drug Enforcement Administration (DEA)
[10] Risk Factors for Opioid Misuse, Addiction, and Overdose – U.S. Department of Labor