The Shocking Truth About Opiate Heroin, Fentanyl Dangers & Recovery
Opioid use disorder and opiate addiction remain at epidemic levels in the US and worldwide. Three million US citizens and 16 million people worldwide have had or currently suffer from opioid use disorder (OUD). More than 500,000 in the US are dependent on heroin. Continue to read more about opiates and opioids effects and addiction treatment.
Clinically Reviewed by Lauren Barry, LMFT, MCAP, QS
Medically Reviewed by Ali Nikbakht, PsyD
Updated on September 20, 2025 — Editorial Policy | Research Policy | Privacy Policy
The Shocking Truth About Opiate Heroin, Fentanyl Dangers & Recovery
Opioid use disorder and opiate addiction remain at epidemic levels in the US and worldwide. Three million US citizens and 16 million people worldwide have had or currently suffer from opioid use disorder (OUD). More than 500,000 in the US are dependent on heroin. Continue to read more about opiates and opioids effects and addiction treatment.
Clinically Reviewed by Lauren Barry, LMFT, MCAP, QS
Medically Reviewed by Ali Nikbakht, PsyD
Reviewed / Updated: September 20, 2025 — Editorial Policy | Research Policy | Privacy Policy
What Makes Opiate Drugs So Dangerous?
Opioid dependence, or opioid addiction, is a long-term disease. It affects the central nervous system and can happen from using opiates for a long time. This dependency leads to withdrawal symptoms when attempting to quit. It commonly starts with prescription pain medications, but may include other illicit drugs like heroin. Opiates are also frequently referred to as narcotics.
Symptoms of opioid addiction vary depending on which drug you were addicted to. The National Institute on Drug Abuse (NIDA) estimates that 1.9 million people in America have opiate addiction. This number keeps growing. People with opiate addiction need to find a treatment center that uses proven methods. Many programs provide referrals and simple instructions on what to expect.
Opioid drug addiction is serious. You should know the symptoms to watch for before it becomes a problem for you or someone you care about. This article will review those symptoms and provide top solutions to help combat addiction.
Opiates List
Is morphine an opiate? Is heroin an opiate? Find out what an opiate is. Here’s a list of some commonly used medications under this class of drugs:
- Morphine: One of the most well-known narcotics. Opiate medication, such as morphine, is often used for severe pain relief, including post-surgical and cancer pain.
- Codeine: Used for moderate pain and as a cough suppressant. Codeine opiate is an opiate often found in combination with other medications.
- Hydrocodone: Frequently prescribed for pain relief, often combined with acetaminophen or ibuprofen.
- Oxycodone: Is oxycodone an opiate? Yes. They are used for moderate to severe pain. They come in different forms, like immediate-release and extended-release options.
- Fentanyl: Is fentanyl an opiate? Yes, fentanyl is a type of opioid painkiller. It is a synthetic compound that works on opioid receptors in the body to relieve pain. Fentanyl is a strong opiate. It is often more powerful than natural narcotics like morphine. Doctors use it to manage severe pain.
- Tramadol: A unique opioid used for moderate to moderately severe pain. It has a lower risk of breathing problems than other opioids.
- Meperidine (Demerol): Used for short-term pain relief, but its use is limited due to potential toxic effects.
- Buprenorphine: Pain management medication and also as a medication-assisted treatment for opioid dependence.
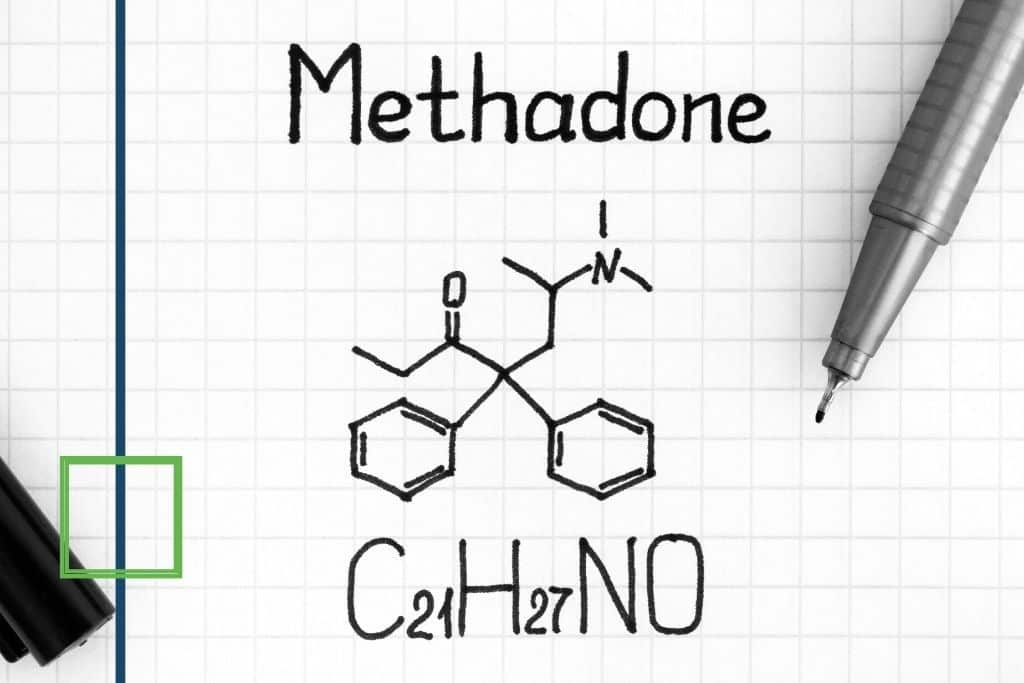
- Methadone: Often used in opioid replacement therapy for opioid dependence and as a pain reliever.
- Hydromorphone: More potent than morphine, often used for severe pain, such as in cancer or postoperative settings.
- Tapentadol: An analgesic with both opioid and non-opioid effects, used for moderate to severe pain.
- Naloxone: While not an opiate, naloxone is an opioid receptor antagonist (opiate receptors; opiate antagonists) that reverses opioid overdoses.
Opiate Analgesic Uses
Opiate painkillers should only be used with a doctor’s guidance and prescription. They can be risky and may lead to dependence.
- Pain Relief: Opiate painkillers are mainly used to treat moderate to severe pain. This includes pain after surgery, injury, or in long-term pain conditions.
- Cancer Pain: They are often prescribed to alleviate pain associated with advanced cancer and terminal illnesses.
- Postoperative Pain: Narcotics can help control pain following surgical procedures.
- Acute Trauma: They may be administered for pain management after accidents or traumatic injuries.
- Severe Back Pain: Narcotics can be used for severe cases of back pain that do not respond well to other treatments.
- Labor Pain: Sometimes, Narcotics may be used during labor to help manage pain.
- Palliative Care: Narcotics are used in hospice and palliative care settings to comfort patients with life-limiting illnesses.
- Cough Suppression: Certain narcotic derivatives are used as cough suppressants in over-the-counter medications.
Opiates Side Effects
It’s crucial to discuss potential side effects and risks with a healthcare provider before using narcotics and to use them only as prescribed.
- Drowsiness.
- Constipation.
- Nausea.
- Vomiting.
- Dry mouth.
- Dizziness.
- Itching.
- Confusion.
- Respiratory depression.
- Low blood pressure.
- Dependence.
- Tolerance.
- Sedation.
- Slurred speech.
- Decreased heart rate.
Symptoms of Opiate Withdrawal
Opiate withdrawal symptoms can vary in intensity based on factors such as the type of narcotics, dosage, and individual differences. Withdrawal from these drugs can be challenging, and seeking medical guidance and support is recommended for a safer and more comfortable process.
- Anxiety: Feelings of restlessness, unease, and worry.
- Insomnia: Difficulty falling asleep or staying asleep.
- Yawning and Runny Nose: Frequent yawning and a runny or stuffy nose.
- Muscle Aches: Pain and discomfort in the muscles and joints.
- Sweating: Excessive sweating and clammy skin.
- Chills: Shivering and cold sensations.
- Nausea and Vomiting: Feeling sick to the stomach and possibly vomiting.
- Diarrhea: Frequent and watery bowel movements.
- Dilated Pupils: Pupils of the eyes may appear larger than usual.
- Goosebumps: Formation of small bumps on the skin resembling “goosebumps.”
- Agitation: Restlessness, irritability, and difficulty staying calm.
- Cravings: Intense desire for the drug.
Opiate Addiction Symptoms
Here’s a simple list of common symptoms associated with narcotics addiction:
- Craving: A strong and persistent desire to use narcotics, often leading to a preoccupation with obtaining and using the drug.
- Loss of Control: Inability to limit or control narcotics use, even with negative consequences.
- Tolerance: Needing increasing amounts of narcotics to achieve the desired effects or experiencing reduced effects with the same dose.
- Withdrawal: Experiencing physical and psychological symptoms when attempting to reduce or stop narcotics use, leading to a cycle of use to avoid withdrawal.
- Neglecting Responsibilities: Prioritizing drug use over crucial work, school, or home obligations.
- Social Isolation: Withdrawing from friends and family in favor of spending time with fellow users or engaging in drug-related activities.
- Loss of Interest: Diminished interest in previously enjoyed activities and hobbies.
- Mood Changes: Frequent mood swings, irritability, anxiety, or depression.
- Financial Strain: Spending excessive money on obtaining drugs often leads to financial difficulties.
- Doctor Shopping: Seeking multiple doctors or prescriptions to obtain more narcotics.
- Legal Issues: Getting involved in legal problems related to drug possession, distribution, or other criminal activities.
- Neglecting Self-Care: Ignoring personal hygiene, nutrition, and overall health due to drug use.
- Risk-Taking Behavior: Engaging in dangerous activities while under the influence of narcotics.
- Denial: Often downplaying the severity of the addiction or avoiding acknowledging its negative impact on one’s life.
- Failed Attempts to Quit: Repeatedly trying to quit or reduce narcotics use.
It’s crucial to recognize these signs and symptoms and seek professional help if you or someone you know is struggling with narcotics addiction. Addiction to these drugs is a severe medical condition that requires appropriate treatment and support for recovery.
Opiate Overdose
Here’s a simple list of common opiate overdose symptoms:
- Slow or Shallow Breathing: Breathing becomes slow, irregular, or shallow.
- Blue Lips or Fingernails: Skin, lips, or nails may turn bluish or pale due to lack of oxygen.
- Extreme Drowsiness: The person may be difficult to awaken or in a stupor.
- Confusion or Disorientation: Confusion, inability to communicate clearly, or not responding appropriately.
- Inability to Wake Up: The person cannot be awakened from sleep or remains unresponsive.
- Pinpoint Pupils: Pupils become very small, resembling pinpoints.
- Limp Body: The person’s body may feel limp or floppy.
- Cold or Clammy Skin: Skin may feel cold, sweaty, or clammy.
- Vomiting: Nausea and vomiting can be life-threatening if the person is unconscious.
- Slurred Speech: Speech may be difficult to understand or incoherent.
- Seizures: In some cases, an overdose can lead to seizures.
- Loss of Consciousness: The person may lose consciousness and become unresponsive.
Suppose you suspect someone is experiencing a narcotic overdose. In that case, it is crucial to seek immediate medical help by calling emergency services (911 or your local emergency number) and administering naloxone if available. Naloxone is an opioid overdose reversal medication that can save lives. Time is of the essence in responding to an overdose, so it’s essential to act quickly.
Main Differences Between Opioid vs Opiate
While these opioids and opiate terms are frequently interchanged, they have distinctions in meaning. The table below explains the difference between opioid and opiate drugs:
| Opiates vs Opioids Categories | Opioids vs Opiates Definition |
| Chemical Composition | Opiates are naturally occurring compounds in the opium poppy plant, whereas opioids can be natural, synthetic, or semi-synthetic substances created in laboratories. |
| Source | The distinction between opiates and opioids can have legal and regulatory implications. Opiates are often subject to specific regulations due to their natural origin. Opioids are a broad term. They include substances that have different levels of control and regulation. This depends on how they are made and their risk for misuse. |
| Potency and Diversity | Opioids are often more potent than opiates due to their ability to engineer and modify chemical structures. Opioids include a wide range of drugs with different strengths and effects. This group has strong synthetic opioids like fentanyl and carfentanil. |
| Medical Use | The distinction between the two can have legal and regulatory implications. This are often subject to specific regulations due to their natural origin. Opioids are a broad term. They include substances that have different levels of control and regulation. This depends on how they are made and their risk for misuse. |
| Legal and Regulatory Perspective | The distinction between the two can have legal and regulatory implications. These are often subject to specific regulations due to their natural origin. Opioids are a broad term. They include substances that have different levels of control and regulation. This depends on how they are made and their risk for misuse. |
Opioid and Opiate Withdrawal Symptoms
Opiates and opioids have similar withdrawal symptoms. These include strong cravings and physical discomfort like nausea and muscle aches. People may also feel psychological distress and other symptoms from their body’s dependence on these drugs.
Here is a more comprehensive list of opioid and opiate withdrawal symptoms:
- Intense cravings for narcotics.
- Nausea and vomiting.
- Diarrhea.
- Muscle aches and pains.
- Sweating and chills.
- Runny nose and watery eyes.
- Yawning.
- Restlessness and agitation.
- Anxiety and irritability.
- Insomnia and sleep disturbances.
- Dilated pupils.
- Goosebumps (piloerection).
- Abdominal cramps.
- Rapid heartbeat (tachycardia).
- High blood pressure.
- Depression.
- Fatigue and weakness.
- Tremors or shaking.
- Decreased appetite.
- Difficulty concentrating.
The severity and length of withdrawal symptoms can vary. This depends on the type of opioid used, the person’s usage history, and their overall health. Withdrawing from opioids and opiates can be very uncomfortable. In some cases, it can also be medically complex. Therefore, it is best to seek medical help and support during withdrawal.
Common Types of Opiates
This list is not exhaustive, as other narcotic derivatives and formulations exist. Generally, here are some common types of opiates:
- Oxycodone (OxyContin, Percocet).
- Hydrocodone (Vicodin, Norco).
- Buprenorphine (Subutex, Suboxone).
- Hydromorphone (Dilaudid).
- Meperidine (Demerol).
- Morphine.
- Codeine.
- Heroin.
- Fentanyl.
- Methadone.
Skip To:
Learn More:
- Opiate Withdrawal Symptoms, Can You Die From Opiate Withdrawal?
- How Long Do Opiates Stay in Your System, Body, Blood, and Urine?
- Opiate Detox Timeline, Withdrawal Symptoms, and Top Treatment Options
- Xanax and Opiate Withdrawal
- Opiate Withdrawal Restlessness
- Mixing Amphetamines And Opiates
- The Fentanyl Epidemic, Fentanyl Deaths, and Why Is Fentanyl So Popular Now?
- What is Heroin? Heroin Drug Facts. Black Tar Heroin Addiction. What Does Heroin Look Like? Heroin Addiction Treatment.
- Morphine Overdose Symptoms
- How Long Does Morphine Stay in Your System?
Risk Factors of Opiate Addiction
Addiction is a complex disorder; not everyone exposed to the following risk factors will develop an addiction. Prevention, education, and early intervention are crucial in addressing opioid addiction. Generally, several risk factors can contribute to the development of opioid addiction, including the following:
- Genetics: A family history of addiction can increase the risk of opioid addiction, suggesting a genetic predisposition.
- Personal or Family History of Substance Use: Individuals with a history of substance abuse, whether opioids or other substances, may be more susceptible to drug addiction.
- Mental Health Conditions: Co-occurring mental health disorders, such as depression, anxiety, or PTSD, can increase the likelihood of turning to opioids as a form of self-medication.
- Social Environment: Living in an environment where drug use is prevalent or having friends or family members who use narcotics can influence an individual’s likelihood of trying and becoming addicted to drugs.
- Trauma or Stress: Experiencing traumatic events or chronic stress can contribute to initiating and continuing drug use.
- Chronic Pain: People with chronic pain may be given narcotics to help manage their pain. This can raise the risk of dependence and addiction.
- Early Exposure: Using drugs at a young age raises the risk of addiction. This is because the brain is still developing.
- Peer Pressure: Pressure from peers to experiment with drugs can lead to initial drug use and potential addiction.
- Lack of Social Support: People without strong social support may use drugs to deal with feelings of loneliness.
- Easy Access: Easy access to opioids, from prescriptions or illegal sources, can lead to addiction.
- Low Socioeconomic Status: Economic factors and limited resource access can contribute to drug use and addiction.
- Prior History of Addiction: Individuals who have successfully overcome addiction to other substances may be at an increased risk of transferring their addictive behaviors to opioids.

Finding Opiate Detox Near Me
Finding the right detox program is a crucial step in your journey to recovery. Take your time to thoroughly research, compare options, and consider seeking guidance from professionals who specialize in addiction treatment.
- Seek Professional Help: Reach out to doctors, addiction experts, or healthcare providers. They can recommend good detox programs that fit your needs.
- Research Accredited Facilities: Find detox centers that are accredited by respected organizations like CARF or the Joint Commission. Accreditation ensures that the facility meets specific standards of care and safety.
- Read Reviews and Testimonials: Research online reviews, testimonials, and ratings from individuals who have undergone medical detox at different facilities. This can provide insights into the quality of care, staff expertise, and overall patient experiences.
- Evaluate Treatment Approaches: Examine different programs’ detox methods, therapies, and holistic approaches. Ensure the program aligns with evidence-based practices and provides comprehensive support, including medical supervision, counseling, and aftercare planning.
We Level Up Opiates Detox Center
At We Level Up, we help people through their opioid detox journey. We focus on the mental, physical, and spiritual aspects of drug abuse. Our skilled doctors, nurses, therapists, and addiction case managers will help you at every step. They will make sure you get complete support during your recovery.
If you or someone you know is having problems with opioid dependence or addiction, please contact our support team. You can reach us at We Level Up. We are here to help you discover the optimal treatment path tailored to your needs. Each call is confidential, and there’s no obligation.
Specialized, Accredited, 5-Star Reviewed, Evidence-based Addiction & Mental Health Programs. Complete Behavioral Health Inpatient Rehab, Detox plus Co-occuring Disorders Therapy.
CALL(844) 597-1011End the Addiction Pain. End the Emotional Rollercoaster. Get Your Life Back. Start Drug, Alcohol & Dual Diagnosis Mental Health Treatment Now. Get Free, No-obligation Guidance by Substance Abuse Specialists Who Understand Addiction & Mental Health Recovery & Know How to Help.
Opiate Definition Drug Facts
Opiate Meaning
Opiates are a type of organic compound. They come from the opium poppy plant or are made in a lab. Opiates are known for their effects on certain opioid receptors in the brain and nervous system.
New evidence shows that opiates relieve pain by attaching to certain receptors in the brain and spinal cord. These are called opioid receptors. Opiates attach to these receptors. This changes how pain signals are sent. It reduces the feeling of pain and changes how the brain reacts to pain.
It can activate the brain’s reward system. This leads to feelings of happiness and emotional relief, which helps with pain relief. However, this mechanism also underlies the potential for tolerance, dependence, and addiction.
The Use of Opiate Conversion Calculator
Opiate conversion calculators are tools used in healthcare. They help providers convert one opioid medication to the same dose of another opioid. These calculators help provide safe and effective pain management. They also reduce the risk of overdose or not getting enough pain relief when switching between different opiates.
How Long Do Opiates Stay in Your System?
The time opioids can be found in your system depends on several factors. These include the type of opiate, the dose, how often you use it, your metabolism, and the kind of drug test used.
Here’s an approximate range for detection times for different kinds of drug tests:
- Urine Test:
- Short-acting drugs (e.g., heroin, codeine): Up to 2-4 days.
- Longer-acting drugs (e.g., morphine, oxycodone): 3-4 days.
- Saliva Test:
- Up to 1-4 days.
- Blood Test:
- Up to 1-3 days.
- Hair Test:
- Up to 90 days (can vary based on hair growth rate and length)
These are general estimates, and detection times can vary based on individual factors. Also, different opioids may have slightly different detection windows.
It’s essential to consult a medical professional for accurate information and guidance, especially if undergoing drug testing for legal or employment-related purposes.
How Long Does Opiate Withdrawal Last?
How long do opiate withdrawals last? The specific drug, individual metabolism, and usage history determine the withdrawal timeline. Here’s a general timeline of withdrawal symptoms:
Opiate Withdrawal Timeline
| 6 to 12 hours | Early withdrawal symptoms may begin within the first day after the last dose, including anxiety, restlessness, yawning, and sweating. |
| 12 to 48 hours | Symptoms often intensify during this period, including muscle aches, abdominal cramps, nausea, vomiting, diarrhea, and increased heart rate. |
| 2 to 4 days | Peak withdrawal symptoms are usually experienced around this time, with intense cravings, flu-like symptoms, and psychological distress. |
| 5 to 7 days | Physical symptoms start to subside, but psychological symptoms like anxiety, depression, and mood swings can persist. |
| 1 to 2 weeks | Many physical symptoms diminish, although psychological symptoms may still be present. Sleep disturbances and fatigue can persist. |
| 2 to 4 weeks | Symptoms continue to improve, with energy levels gradually returning to normal and mood stabilizing. |
| Beyond 4 weeks | Lingering psychological symptoms may persist, including cravings, depression, and anxiety, which can vary in duration and severity. |
What are Opiates?
Narcotics are potent drugs known for relieving pain and producing a sense of euphoria. The top five opiates examples:
- Morphine: Morphine is a well-known and old narcotic. It is a strong pain reliever used in hospitals for severe pain.
- Codeine: Is codeine an opiate? Yes. Codeine is often used as a milder pain reliever and cough suppressant. It is found in some prescription medications and can be combined with other drugs.
- Heroin: Heroin is an illegal and very addictive drug made from morphine. It is known for its strong euphoric effects and serious health risks.
- Oxycodone: A semi-synthetic drug found in prescription medications like OxyContin and Percocet, oxycodone is prescribed for moderate to severe pain relief.
- Hydrocodone: This is a semi-synthetic drug found in medicines like Vicodin and Norco. It is used to treat pain. Like oxycodone, hydrocodone can lead to dependence and abuse.
How Long Do Opiates Stay in Urine?
These drugs can usually be found in urine tests for 2 to 4 days after use. This depends on the drug, the dose, and how a person’s body processes it. Short-acting drugs like heroin and codeine are found in the body for a shorter time. In contrast, longer-acting drugs like morphine and oxycodone can be detected for a longer period.
The Truth About Rapid Opiate Detox
Rapid opioid detox is a procedure that speeds up withdrawal while the patient is under anesthesia. It is controversial because of possible risks, little proof of long-term success, and high costs. While this method promises quick results, people should be careful. They should research the benefits and risks. It is also important to seek advice from medical professionals.
Is Suboxone an Opiate?
Suboxone is a medication used to treat opioid dependence, and it contains two active ingredients: buprenorphine and naloxone. Buprenorphine, one of the components in Suboxone, is a partial opioid agonist. It activates opioid receptors in the brain but to a lesser extent than full agonists like heroin or oxycodone. Suboxone has an opioid component called buprenorphine. Its formula helps manage cravings and withdrawal symptoms. It also lowers the risk of misuse and overdose linked to regular opioids.
The Use of Clinical Opiate Withdrawal Scale
The Clinical Opiate Withdrawal Scale (COWS) is a tool used by healthcare workers. It helps measure how severe opioid withdrawal symptoms are in people going through detox. It looks at different physical and mental withdrawal symptoms. These include sweating, restlessness, pupil size, and stomach issues. Each sign gets a score. The COWS helps guide treatment decisions, monitor progress, and effectively tailor interventions to manage withdrawal symptoms.

Get Your Life Back
Find Hope & Recovery. Get Safe Comfortable Detox, Addiction Rehab & Dual Diagnosis Trused Care.
7/365 Line (844) 597-1011Opiate vs Opioid Statistics
Illicitly manufactured fentanyl and other synthetic opioids are often more potent than natural opiates, such as morphine or heroin. Even a tiny amount of fentanyl can lead to a lethal overdose. This heightened potency increases the risk of accidental overdose, especially when these potent substances are mixed with other drugs.
128
In 2018, an estimated 128 people died daily in the US from an opioid overdose.
Source: CDC
90,000
More than 90,000 people died from drug overdoses in the US in the year ending September 2020. Opioids played a big role in these deaths.
Source: CDC
10.3 Million
In 2020, about 10.3 million people misused prescription opioids. Of these, 9.9 million misused pain relievers. Additionally, 808,000 people used heroin.
Source: CDC
Top 5 Opiate Studies with Insights
Here’s a patient-friendly chart of the top five opiate studies/guidelines.
Here is a helpful list of the top 5 trusted opiate studies and guidelines. You can use these in clinical documents, program pages, or treatment guides. Each row distills what the evidence implies for treatment and turns it into actionable tips for care teams and admissions scripts. Sources were chosen for recency, rigor, and relevance to integrated treatment.
| Study | Treatment Implications | Insights for Patients |
|---|---|---|
| Randomized trial: Buprenorphine/Naloxone vs Methadone in chronic pain + opioid addiction View Study | Both methadone and buprenorphine/naloxone are effective for pain and addiction; methadone may be more effective for current pain intensity. | Patients with chronic pain and opioid addiction have safe treatment options; discuss goals (e.g., pain relief vs side effects) with your provider. |
| Meta-analysis of opioid maintenance in patients with opioid + cocaine use View Resource | High-dose methadone may be preferable over buprenorphine for patients with co-occurring cocaine use. | If you use more than one substance, treatment may need to be tailored—be open about all drug use with your care team. |
| Detox methods for opiate-dependent adolescents Read Article | Maintenance treatment (not just detox) may be better for adolescents to stay in treatment and prevent relapse. | Young people need longer support—not just a short detox. Maintenance therapy may feel hard, but it improves long-term outcomes. |
| Buprenorphine vs Clonidine in opioid detox for adolescents Read Study | Buprenorphine is more effective than clonidine for keeping adolescents in detox programs and encouraging ongoing care. | If you’re a teen or parent, ask about buprenorphine—it’s safer and more effective than older drugs like clonidine. |
| Review of opioids for chronic pain (U.S. clinical data) Read Review | Long-term opioid use for pain must be balanced with risks of overdose and dependence; not all patients will benefit. | If you’re using opioids for pain, review your treatment regularly; alternatives may help reduce dose and risk. |
The Use of Clonidine for Opiate Withdrawal
Clonidine, an alpha-2 adrenergic agonist, is sometimes used off-label to mitigate specific symptoms during opioid withdrawal.
When someone uses opioids, the body’s natural control of neurotransmitters gets disrupted. This causes more norepinephrine to be released. As a result, people may experience symptoms like anxiety, agitation, and a faster heart rate during withdrawal.
Clonidine works by stimulating alpha-2 adrenergic receptors in the brainstem, reducing the release of norepinephrine, and dampening the activity of the sympathetic nervous system. This mechanism helps reduce some physical and mental symptoms of opioid withdrawal. It makes it easier for people to detox from opioids.
FDA-Approved Opiate Withdrawal Medication
Several medications have been FDA-approved for managing opioid withdrawal symptoms and opioid use disorder. Here are a few medicines commonly used for opiate withdrawal and opioid use disorder treatment:
- Buprenorphine: The FDA has approved buprenorphine to treat opioid use disorder. It is a partial opioid agonist. It can help manage withdrawal symptoms and cravings. It has various forms, including sublingual tablets, films, and implants.
- Methadone: This is a medication approved by the FDA for treating opioid use disorder. Methadone is a full opioid agonist. It can help lessen withdrawal symptoms and cravings. It is typically administered under strict medical supervision in specialized clinics.
- Naltrexone: Available in oral and extended-release injectable forms (Vivitrol), naltrexone is an opioid receptor antagonist that blocks the effects of opioids. It prevents relapse in individuals who have already detoxified from opioids.
- Clonidine: Clonidine is not specifically approved by the FDA for opioid withdrawal. However, it is sometimes used off-label. It can help manage symptoms like anxiety, agitation, and sweating during withdrawal.
- Lofexidine: Lofexidine (Lucemyra) is FDA-approved for managing opioid withdrawal symptoms. It can help reduce the severity of withdrawal symptoms, but does not treat the underlying opioid use disorder.
These medications are typically part of comprehensive treatment plans, including counseling, therapy, and support services. Treatment decisions should be made in consultation with a healthcare provider based on individual needs and circumstances.
FAQs
-
How long does opiates stay in your system?
The time these drugs stay in your body can change. It depends on the type of drug, your metabolism, the dose, and how often you use it. Opioids can usually be found in urine for 2 to 4 days. However, this time can be shorter or longer based on different factors.
-
Why do opiates make you itch?
This class of drugs can cause itching due to their effects on histamine release in the body. They cause the release of histamine. This compound helps the body’s immune response. It can lead to skin irritation and itching, especially in sensitive people.
-
Is Percocet an opiate?
Yes, Percocet is an opioid pain medication that contains two active ingredients: oxycodone and acetaminophen. Oxycodone is a man-made opioid. It works on the same brain receptors as natural opiates. This helps relieve pain. Acetaminophen boosts its pain-relieving effects.
-
Can you die from opiate withdrawal?
While withdrawal is usually not deadly, severe symptoms can cause problems. These problems may be life-threatening, especially for those with existing health issues. It’s essential to seek medical supervision and support during withdrawal, especially in cases of heavy and prolonged drug use.
-
How long does Suboxone block opiates?
Suboxone, a medication used to treat opioid dependence, contains buprenorphine and naloxone. Buprenorphine is the active ingredient. It has a longer half-life than most full opioid agonists. This allows it to block opioid receptors for about 24 to 60 hours. The exact time can vary based on individual factors. Naloxone is included to deter misuse and is generally inactive when Suboxone is taken as prescribed.
Get Help. Get Better. Get Your Life Back.
Searching for Accredited Drug and Alcohol Rehab Centers Near You?
Even if you have failed previously and relapsed, or are in the middle of a difficult crisis, we stand ready to support you. Our trusted behavioral health specialists will not give up on you. When you feel ready or just want someone to speak to about therapy alternatives to change your life call us. Even if we cannot assist you, we will lead you to wherever you can get support. There is no obligation. Call our hotline today.
(844) 597-1011Top-Rated Opiate Detox and Addiction Treatment at We Level Up
We Level Up treatment centers stand ready to support people suffering from addiction. As a certified rehabilitation center, we are here to help you reach your goals, one step at a time.
To aid you in achieving and sustaining sobriety, we prioritize a tailored approach to treatment. From the start of your time with us, our counselors will help you create a plan. This plan will match your health, the substances you use, your daily life, your preferences, and your unique needs.
If you are considering addiction treatment for yourself or someone you love, We Level Up can help. Contact us today for a confidential consultation with a member of our intake team. We can help you explore treatment options, and each call is confidential.
The opioid detox process is a critical step in overcoming opioid addiction. It allows the body to eliminate opioids while managing withdrawal symptoms and preparing for ongoing addiction treatment. Here’s an in-depth overview of the opioid detox process:
- Assessment and Preparation: Before detox starts, individuals have a thorough evaluation. This checks their medical history, opioid use, overall health, and any other conditions. A treatment plan is created based on this assessment. It looks at factors like the type of opioids used, how long they were used, and the person’s overall health.
- Medical Supervision: Opioid detox is often conducted under medical supervision to ensure safety and minimize discomfort. Medical professionals monitor vital signs, assess withdrawal symptoms, and administer medications if necessary.
- Tapering: In some cases, a gradual reduction of opioid dosage, known as tapering, is used to minimize withdrawal symptoms. This approach helps the body adjust to decreasing levels of opioids over time.
- Medication-Assisted Treatment (MAT): Some medications, like methadone, buprenorphine, or naltrexone, can help during detox. They manage withdrawal symptoms and cravings. MAT can help individuals transition more comfortably through the detox process.
- Withdrawal Phase: As opioids are gradually eliminated from the body, withdrawal symptoms begin. These symptoms can include anxiety, restlessness, sweating, muscle aches, nausea, vomiting, diarrhea, and insomnia. The severity and length of withdrawal symptoms can vary. This depends on the type of opioids used and the person’s body.
- Medical Management: Medical professionals provide supportive care and medication to alleviate withdrawal symptoms. Medications may include non-opioid pain relievers, anti-nausea drugs, and medications to address specific symptoms.
- Psychological Support: Counseling and therapy are essential components of opioid detox. Behavioral therapies help individuals cope with cravings, address underlying issues, and develop strategies for relapse prevention.
- Nutrition and Hydration: Good nutrition and hydration are important during detox. They help the body heal and reduce physical discomfort.
- Emotional Support: Emotional support from medical staff, therapists, and peers can help individuals navigate the emotional challenges of detoxification.
- Transition to Treatment: Detox is often the initial phase of a comprehensive addiction treatment plan. Following detox, individuals are encouraged to continue with addiction treatment, including residential or outpatient rehab, counseling, therapy, and ongoing support.
Detox is the first step in recovering from opioid addiction. The main goal is to tackle the root causes of addiction. We also want to create plans to stay sober for a long time. A personalized and complete approach is key for each person’s needs. This is important for a successful opioid detox and recovery journey.
Medication-Assisted Treatment for Addiction
Medication-Assisted Treatment (MAT) for opioid addiction uses FDA-approved medicines. These include methadone, buprenorphine, and naltrexone. MAT also includes counseling and behavioral therapies to help with opioid use disorder. MAT helps individuals manage withdrawal symptoms, reduce cravings, and normalize brain function, allowing for a comprehensive approach to recovery.
Behavioral Therapies in Inpatient Program
Behavioral therapies for opioid addiction encompass a range of therapeutic approaches designed to address the psychological and behavioral aspects of opioid use disorder. These therapies modify unhealthy thought patterns and behaviors, develop coping skills, and promote sustainable recovery. Examples include Cognitive-Behavioral Therapy (CBT), Contingency Management, Motivational Interviewing, and 12-Step Facilitation. These methods can be adjusted to fit a person’s needs and situation.
Aftercare Programs for Long-Term Sobriety
Aftercare programs following opioid addiction treatment are crucial for maintaining long-term recovery. These programs provide support, resources, and strategies. They help people avoid relapse and deal with daily life challenges. Typical components of aftercare programs include:
- Support groups.
- Individual counseling.
- Continued medication management (if applicable).
- Relapse prevention planning.
- Vocational and educational support.
- Connections to community resources.
First-class Facilities & Amenities
Trusted Integrated Addiction & Mental Health Rehabilitation Treatment
Rehab Centers TourEstablished Addiction Centers. Serene Private Facilities. Inpatient rehab programs vary.
Addiction Helpline (844) 597-1011Comprehensive recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Success Stories Across Our Network
- Low Patient to Therapist Ratio
- Onsite Medical Detox Center
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Alumni Coaching, Recovery & Personal Development Events
What are the Top 10 FAQs Opiate Drugs?
-
Is Tramadol an opiate?
Tramadol is an opioid pain medication that acts on the brain’s opioid receptors, making it practical for pain relief. Tramadol opiate has unique properties and mechanisms compared to traditional opiates like morphine or heroin.
-
Does Gabapentin help with opiate withdrawal?
Gabapentin is sometimes used off-label to help manage specific symptoms of opioid withdrawal, such as anxiety, restlessness, and sleep disturbances. However, the use of Gabapentin for opiate withdrawal and its effectiveness can vary from person to person. Consulting a medical professional for proper guidance and supervision during withdrawal is essential.
-
Is methadone an opiate?
Yes, methadone is an opioid medication often used to treat opioid addiction. It works on the same opioid receptors in the brain as other opiates. This helps relieve withdrawal symptoms and reduces cravings for stronger opioids like heroin.
-
Is Kratom an opiate?
Kratom is not classified as an opiate but interacts with the same receptors in the brain that opioids target. Kratom opiate-like effects are the reason why some people use it to relieve pain or manage withdrawal symptoms. Still, the safety and efficacy of Kratom for opiate withdrawal are subjects of ongoing research and debate.
-
Is cocaine an opiate?
No. It is a strong stimulant drug. It affects the central nervous system. It causes intense happiness, more energy, and greater alertness.
-
Is hydrocodone an opiate?
Yes. It is a semi-synthetic opioid medication for pain relief and cough suppression. It binds to the brain’s opioid receptors, producing analgesia and, in some formulations, antitussive effects.
-
Is Xanax an opiate?
No. It is a benzodiazepine medication primarily prescribed for treating anxiety and panic disorders. Benzodiazepines work on different receptors in the brain than opiates and have distinct mechanisms of action.
-
Is meth an opiate?
No, methamphetamine (meth) is not an opiate. It is a potent central nervous system stimulant that increases energy, focus, and euphoria. Is methamphetamine an opiate? No. Opiates, on the other hand, are a class of drugs derived from the opium poppy plant and are used for their pain-relieving and sedative effects. More questions about “meth opiate?” Head on to methamphetamine addiction.
-
Is Dilaudid an opiate?
Yes, Dilaudid (generic name: hydromorphone) is an opiate. It is a potent opioid analgesic prescribed for severe pain management, working by binding to the brain’s opioid receptors to alleviate pain.
-
Is Valium an opiate?
No. It is a benzodiazepine medication for anxiety, muscle spasms, and seizures. Opiates and benzodiazepines are two types of drugs. They work in different ways and affect the brain differently.
How Long Do Opiates Stay in Your System? How Long Do Opiates Stay in Urine, Blood, & Body?
Opiates can typically be detected in a person’s urine for about 2 to 4 days after use. The detection window depends on several factors. These include the type of drug, the person’s metabolism, how often they use it, and how sensitive the drug test is. Certain drugs and metabolites may be detectable for up to a week or more.
If you or a loved one is struggling with opioid addiction or other substance use disorder(s), call for a FREE consultation 24/7 at (561) 678-0917
Get FREE addiction treatment insurance check – https://welevelup.com/rehab-insurance/
How Long Do Opiates Stay in Your System? Video Transcript.
About We Level Up treatment centers:
We’re a leading nationwide network of substance abuse and mental health treatment centers. We Level Up addiction centers have helped thousands of clients. They struggle with drug addiction, alcohol addiction, and mental health issues. We Level Up offers first-class facilities and amenities. World-class, high-quality addiction & Mental health rehabilitation treatment. With renowned accredited centers in serene private facilities.
Welcome to the We Level Up treatment center video series.
The time narcotics stay in your system depends on the type of drug, the dose, and how often you use it. Generally, narcotics can stay in your system for two to four days. However, heavier and chronic users may have residues in their system for up to seven days.
Narcotics can be detected in the blood test for up to 24 hours and the urine test for up to three days. Narcotics can be detected in the hair follicles for up to 90 days. Narcotics can stay in the body for up to 30 days or more in chronic users.
Narcotics often have short half-lives, meaning their effects can linger for several hours even though they swiftly leave the body. However, Opioids can linger in a person’s bloodstream for several hours or days after the symptoms subside, depending on the substance used. Urine tests, one of the more common types of drug testing, can identify opioid usage for extended periods, often up to three to four days, and some tests can identify opioid use for up to three months.
What are Opioids?
Opioids, sometimes called narcotics, are medications to treat persistent or severe pain. People use them for many reasons. They help those with constant headaches and high blood alcohol levels. They also aid recovery after surgery. They can ease severe pain from cancer. Adults and kids use them after serious injuries from sports, falls, car accidents, or other events.
A large class of painkillers known as opioids interacts with opioid receptors in your cells to relieve pain. Opioids can be made in a lab, like fentanyl, or from poppy plants, like morphine. Other examples include Kadian, Ms. Contin, Actiq, and Duragesic.
Your brain cells release signals that reduce your sense of pain and increase your emotions of pleasure when opioid drugs pass through your blood and bind to opioid receptors. Opioid addiction can happen after just a week of use. The risk for long-term opioid abuse increases after only five days of taking medicine. Some individuals who only intended to use opioids for a week have continued to do so a year later.
Compared to 2019, the age-adjusted rate of drug overdose deaths rose to 31% in 2020. Young people aged 15 to 24 had the biggest rise in deaths. Adults aged 35 to 44 had the highest rates of drug overdose deaths. The fight against substance use disorders and the opioid pandemic must continue in all facets.
Opioid Drug Names
There are a variety of narcotics, all with different names. Some examples include codeine, morphine, oxycodone, hydrocodone, fentanyl, and methadone. It is crucial to know the names of drugs when seeking help for addiction, as intervention strategies and treatment plans may depend on the substances being abused.
Experience Transformative Recovery at We Level Up Treatment Centers.
See our authentic success stories. Get inspired. Get the help you deserve.



Start a New Life
Begin with a free call to an addiction & behavioral health treatment advisor. Learn more about our dual-diagnosis programs. The We Level Up Treatment Center Network delivers recovery programs that vary by each treatment facility. Call to learn more.
- Personalized Care
- Caring Accountable Staff
- World-class Amenities
- Licensed & Accredited
- Renowned w/ 100s 5-Star Reviews
We’ll Call You
Search We Level Up Opiates Detox, Mental Health Topics & Resources
Resources
Opiate withdrawal – Covering symptoms, timeline, and treatment options.
Morphine opiate addiction – Explains signs, risks, and treatment for morphine abuse.
Opiate overdose reversal – Narcan and naloxone for saving lives from opiate overdoses.
Black tar opiate risks – Details about heroin as an opiate and its harmful effects.
Sources
[1] Dydyk AM, Jain NK, Gupta M. Opioid Use Disorder. [Updated 2022 Jun 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553166/
[2] Azadfard M, Huecker MR, Leaming JM. Opioid Addiction. [Updated 2023 Jan 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448203/
[3] Clinical Guidelines for Withdrawal Management and Treatment of Drug Dependence in Closed Settings. Geneva: World Health Organization; 2009. 4, Withdrawal Management. Available from: https://www.ncbi.nlm.nih.gov/books/NBK310652/
[4] Institute of Medicine (US) Committee on Opportunities in Drug Abuse Research. Pathways of Addiction: Opportunities in Drug Abuse Research. Washington (DC): National Academies Press (US); 1996. B, Drug Abuse Research in Historical Perspective. Available from: https://www.ncbi.nlm.nih.gov/books/NBK232965/
[5] Opioid Withdrawal – U.S. Department of Health and Human Services National Institutes of Health Available from: https://medlineplus.gov/ency/article/000949.htm
[6] Prescription Opioids DrugFacts – National Institute on Drug Abuse (NIDA)
[7] Understanding the Opioid Overdose Epidemic – Centers for Disease Control and Prevention (CDC)
[8] Schiller EY, Goyal A, Mechanic OJ. Opioid Overdose. [Updated 2022 Sep 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470415/
[9] Narcotics (Opioids) – Drug Enforcement Administration (DEA)
[10] Risk Factors for Opioid Misuse, Addiction, and Overdose – U.S. Department of Labor