Dangers of Mixing Antibiotics and Alcohol
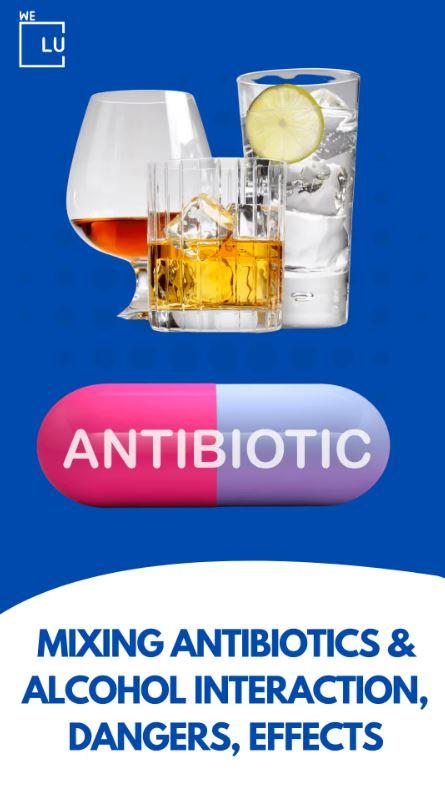
The concurrent use of antibiotics and alcohol can pose potential dangers due to the interaction between these substances. Certain antibiotics, such as metronidazole and tinidazole, inhibit the enzyme aldehyde dehydrogenase, which is involved in alcohol metabolism. As a result, when alcohol is consumed while taking these antibiotics can lead to a buildup of acetaldehyde. This toxic substance causes unpleasant symptoms such as facial flushing, rapid heartbeat, nausea, and headache. Known as the disulfiram-like reaction, it can be highly uncomfortable and, in rare cases, may even result in loss of consciousness.
Moreover, alcohol consumption while on antibiotics can potentially compromise the effectiveness of the medication in treating the underlying infection or condition. Alcohol can impair the immune system, hinder the body’s healing processes, and increase the risk of adverse antibiotic reactions.
To ensure safety and optimize the therapeutic outcomes of antibiotics, it is generally advised to abstain from alcohol consumption while taking these medications. Consulting with a healthcare professional is necessary for advice, as the specific interactions between antibiotics and alcohol may vary based on the type of antibiotic and individual factors.
Antibiotics and Alcohol Myth
For decades, doctors and pharmacists have advised staying away from alcohol when taking prescription antibiotics. This advice may have originated in the 1950s when penicillin became the first effective treatment for sexually transmitted infections (STIs) such as syphilis and gonorrhea.
Physicians were worried that alcohol intoxication could undo their expensive treatment with the new miracle drugs. So patients were advised to abstain from alcohol until things cleared up. This may be well-founded because patients receiving penicillin for STD (sexually transmitted disease) at that time were more likely to engage in risky sexual activity while intoxicated.
The advice that you shouldn’t mix antibiotics and alcohol does hold for a small group of anti-infective drugs, including metronidazole (Flagyl, Metronide, or Metrogyl), tinidazole (Fasigyn or Simplotan), and sulfamethoxazole/trimethoprim (Bactrim, Co-trimoxazole). The side effects of both Bactrim and alcohol are similar, including stomach upsets, dizziness, and drowsiness. Mixing Bactrim and alcohol can increase the side effects, making the person extremely uncomfortable.
These antibiotics block one of the significant pathways that metabolize alcohol and cause a rapid build-up of acetaldehydes, which are responsible for many of the uncomfortable physical effects of hangovers. With these antibiotics, you can be red-faced, fainting, and vomiting after as little as one glass of beer.
What Happens If You Drink Alcohol While Taking Antibiotics?
Drinking alcohol while taking antibiotics can lead to various adverse effects and potential risks.
- Reduced Effectiveness of Antibiotics: Alcohol can interfere with the effectiveness of antibiotics in treating the underlying infection or condition. It may hinder the antibiotic’s ability to kill bacteria or inhibit their growth, potentially prolonging recovery.
- Increased Risk of Side Effects: Alcohol can intensify the side effects of certain antibiotics, making them more pronounced or severe. This can include dizziness, drowsiness, nausea, vomiting, diarrhea, and stomach upset.
- Potential Drug Interactions: Alcohol can interact with antibiotics, leading to unpredictable reactions or interactions. These interactions may vary depending on the specific antibiotic and individual factors, potentially causing harm or reducing the effectiveness of the medication.
- Disulfiram-Like Reaction: Some antibiotics, such as metronidazole and tinidazole, can trigger a disulfiram-like reaction when combined with alcohol. This reaction produces symptoms like facial flushing, rapid heartbeat, nausea, vomiting, headache, and overall discomfort.
- Liver Strain: Both alcohol and certain antibiotics can put a strain on the liver. Combining them may increase the risk of liver damage or compromise the liver’s ability to process the medication and detoxify the body.
To ensure the safe and effective use of antibiotics, it is generally recommended to abstain from alcohol consumption while taking these medications.
Skip To:
Learn More:
- Can You Drink Alcohol With Antibiotics Amoxicillin? Amoxicillin and Alcohol Interactions. Can You Drink on Amoxicillin? Amoxicillin Alcohol Effects. Amox CLAV and Alcohol.
- Can You Take Ibuprofen With Alcohol? Can You Mix Alcohol and Ibuprofen? Will Ibuprofen and Alcohol Kill You? Ibuprofen and alcohol Effects Exposed. Alcohol and Ibuprofen Dangers.
- Azithromycin and Alcohol, Risks and Effects
- Bactrim and Alcohol Death, Trimethoprim and Sulfamethoxazole Side Effects with Alcohol
- Mixing Steroids and Alcohol Dangers. Can You Drink Alcohol on Steroids? Alcohol with Steroids Interactions.
- Risks of Mixing Prescription Drugs With Alcohol
- Alcohol Detox Timeline & How To Safely Manage Alcohol Withdrawal Symptoms Treatment
- Alcohol Addiction Treatment, Alcoholism, Signs, Complications & Recovery Rehab Programs
Alcohol and Antibiotics Interaction
The specific interactions between antibiotics and alcohol can vary, and it is always best to consult with a healthcare professional or read the medication’s instructions and warnings. However, here is a list of some commonly used antibiotics and their general warnings or precautions regarding alcohol:
| Metronidazole (Flagyl) | Combining metronidazole with alcohol can cause a severe disulfiram-like reaction, leading to flushing, rapid heartbeat, nausea, vomiting, and headache. It is strongly advised to avoid alcohol consumption while taking metronidazole and for at least 48 hours after completing the medication. |
| Tinidazole | Like metronidazole, tinidazole can also cause a disulfiram-like reaction when combined with alcohol. It is recommended to refrain from alcohol use during tinidazole treatment and for at least 72 hours after completing the medication. |
| Linezolid (Zyvox) | Linezolid has the potential to interact with alcohol, leading to an increase in blood pressure and potential serotonin syndrome. It is generally recommended to avoid alcohol while taking linezolid. |
| Oxazolidinones | Oxazolidinones like Linezolid shouldn’t be mixed with alcohol because they can cause fever, agitation, rapid heartbeat, unusual sweating, rapid breathing, vomiting, elevated blood pressure, seizures, abnormal heart rhythm, coma, cardiorespiratory depression, muscle spasms, muscle rigidity, and affect mental health. |
| Trimethoprim/Sulfamethoxazole (Bactrim, Septra) | While alcohol may not directly interact with trimethoprim/sulfamethoxazole, both substances can individually cause stomach upset and gastrointestinal symptoms. It is advisable to use caution and moderate alcohol consumption while taking this antibiotic. |
| Tetracyclines | Alcohol should be avoided when taking antibiotics like tetracyclines, including doxycycline and minocycline, because doxycycline reduces the effectiveness of antibiotics, and minocycline can increase liver disease risks. |
| Fluoroquinolones | Fluoroquinolones like levofloxacin and ciprofloxacin can cause confusion, nervousness, agitation, memory loss, disorientation, and attention disturbances when mixed with alcohol. The effects are, however, amplified with high alcohol consumption. |
| Sulfonamides | Sulfonamides like trimethoprim and sulfamethoxazole shouldn’t be mixed with alcohol to avoid side effects like a folic acid deficiency. |
| Nitroimidazoles | Nitroimidazoles, like metronidazole, can cause headaches, facial flushing, nausea, vomiting, and abdominal cramping when mixed with alcohol. You shouldn’t take alcohol for three days after your last dose of Nitroimidazoles. |
Antibiotic and Alcohol Drug Facts
Does Alcohol Affect Antibiotics?
Antibiotics are common agents used in modern healthcare. These compounds target bacteria and are intended to treat and prevent bacterial infections.
Combining antibiotics and alcohol will not usually lower your antibiotic’s effectiveness, but it may cause side effects and hinder your body’s natural ability to heal itself. Drinking alcohol while fighting an infection can lead to the following:
- Upset stomach and dehydration.
- Lower your immune response.
- Interrupt normal sleep.
Some antibiotics can also harm your liver, so you must check with your doctor or pharmacist before mixing alcohol with prescription drugs.
Can You Drink Alcohol With Antibiotics Amoxicillin?
It is considered safe to consume moderate amounts of alcohol while taking amoxicillin, as no specific interaction poses a significant risk. However, it is always recommended to follow the instructions and advice provided by your doctor.
How Long After Taking Antibiotics Can You Drink Alcohol?
The specific antibiotic and individual factors determine the recommended time to wait before consuming alcohol after taking antibiotics. However, as a general guideline:
Completion of Antibiotic Course
- It is advisable to wait until you have completed the prescribed antibiotics.
- Completing the treatment ensures that the infection is properly treated and reduces the risk of complications.
Allow Sufficient Time
- After completing the antibiotic course, it is generally recommended to wait at least 24 to 48 hours before consuming alcohol.
- Allow enough time for the antibiotics to be metabolized and eliminated from the body.
However, some antibiotics may have a longer duration of action or potential interactions with alcohol, requiring a longer waiting period.
Can I drink alcohol while on antibiotics? To ensure the safest and most effective use of antibiotics, it is always best to consult with a healthcare professional for personalized advice regarding alcohol consumption after completing the antibiotic treatment. They can provide specific guidance based on your circumstances.
Harmful Interactions of Mixing Alcohol With Medicines Free PDF
Download the file below about different medicines you should not mix with alcohol. The National Institute on Alcohol Abuse and Alcoholism (NIAAA) made this printable pdf available and free to download in raising awareness about the dangers of alcohol drinking.

Get Your Life Back
Find Hope & Recovery. Get Safe Comfortable Detox, Addiction Rehab & Dual Diagnosis High-Quality Care.
Hotline(844) 597-1011Antibiotics Alcohol-Related Statistics
Polysubstance abuse refers to concurrently using or abusing multiple substances, such as alcohol and drugs. When alcohol is combined with other substances, including illicit drugs, prescription medications, or over-the-counter drugs, it can significantly increase the risks and dangers associated with substance use disorders.
30%
Annually, roughly 30% of emergency department visits are related to the misuse of prescriptions with alcohol.
Source: NCBI
47%
Among adult US citizens who reported alcohol use, 47% used prescription drugs concurrently. This emphasizes the possibility of interactions between alcohol and prescription drugs.
Source: NCBI
17 Million
Alcohol is the most abused habit-forming substance in the US. More than 17 million US citizens are considered to suffer from addiction to alcohol.
Source: NCBI
What Are The Antibiotics That You Can Drink Alcohol With?
Can you have alcohol with antibiotics? Several antibiotics can be safely consumed with moderate amounts of alcohol, as they do not have specific interactions that pose significant risks. However, individual factors and personal health conditions can influence the safety of combining antibiotics with alcohol. It is always suggested to consult with your doctor or read the medication’s instructions and warnings for specific guidance if you are taking antibiotics and plan to drink alcohol.
Get Help. Get Better. Get Your Life Back.
Searching for Accredited Drug and Alcohol Rehab Centers Near You?
Even if you have failed previously and relapsed, or are in the middle of a difficult crisis, we stand ready to support you. Our trusted behavioral health specialists will not give up on you. When you feel ready or just want someone to speak to about therapy alternatives to change your life call us. Even if we cannot assist you, we will lead you to wherever you can get support. There is no obligation. Call our hotline today.
(844) 597-1011Side Effects Of Antibiotics With Alcohol
Alcohol is also considered a central nervous system (CNS) depressant. Some antibiotics, like metronidazole (Flagyl), may also lead to CNS side effects such as sedation, dizziness, and confusion.
When alcohol is combined with antibiotics that also have a CNS depressant effect, additive effects may occur. These effects can be severe when driving or operating machinery, in the elderly, and in patients who may take other CNS depressant medications, such as opioid pain relievers, muscle relaxants, antidepressants, and anxiety or seizure medications.
Antibiotics and Alcohol Stomach Side Effects
Stomach problems, such as nausea, vomiting, diarrhea, and stomach pain, can be expected with antibiotics, too. Consuming alcohol can worsen these stomach side effects.
Antibiotics and Alcohol Liver damage
Can I drink alcohol with antibiotics? Excessive alcohol use is well-known to cause liver damage like cirrhosis. Taking antibiotics that can also damage the liver may worsen these problems.

First-class Facilities & Amenities
World-class High-Quality Addiction & Mental Health Rehabilitation Treatment
Rehab Centers TourRenowned Addiction Centers. Serene Private Facilities. Inpatient rehab programs vary.
Addiction Helpline(844) 597-1011Proven recovery success experience, backed by a Team w/ History of:
15+
Years of Unified Experience
100s
5-Star Reviews Across Our Centers
10K
Recovery Success Stories Across Our Network
- Low Patient to Therapist Ratio
- Onsite Medical Detox Center
- Comprehensive Dual-Diagnosis Treatment
- Complimentary Family & Alumni Programs
- Coaching, Recovery & Personal Development Events
Alcohol Antibiotics Misuse and Abuse Treatment
Mixing antibiotics and alcohol can lead to risky behavior, such as addiction, and harmful side effects. For worst-case scenarios, the combination of antibiotics and alcohol increases the risk of overdose. Not only can alcohol interact badly with some medications and cause severe side effects, but it can also potentially interrupt the natural healing process.
People with a history of problem drinking and alcohol dependence will need to inform their doctor about these problems when they take antibiotics. Furthermore, these individuals must get help from a qualified addiction rehabilitation center.
Polysubstance abuse is the consumption of more than one substance simultaneously. While some drug users have a preferred drug, others have several drugs they like to take. Polysubstance abuse is common, and these drug users are clinically classified as having multiple comorbid substance disorders. Because withdrawal from various substances is more complicated than withdrawal from one substance, inpatient medical detox is generally recommended. Treatment aims to restore some or all normal liver functioning by addressing the underlying problem of polysubstance abuse.
Contact We Level Up alcohol rehab center to get started. We can help you explore different treatment options and provide resources.
World-class, Accredited, 5-Star Reviewed, Effective Addiction & Mental Health Programs. Complete Behavioral Health Inpatient Rehab, Detox plus Co-occuring Disorders Therapy.
CALL(844) 597-1011End the Addiction Pain. End the Emotional Rollercoaster. Get Your Life Back. Start Drug, Alcohol & Dual Diagnosis Mental Health Treatment Now. Get Free No-obligation Guidance by Substance Abuse Specialists Who Understand Addiction & Mental Health Recovery & Know How to Help.
Top 3 Can You Drink Alcohol While Taking Antibiotics? FAQs
-
Can I drink alcohol while taking antibiotics?
It is generally advisable to avoid mixing antibiotics and alcohol. While some antibiotics may not have direct interactions with alcohol, consuming alcohol can potentially interfere with the effectiveness of the medication and increase the risk of side effects.
-
Can you drink alcohol on antibiotics?
Avoid drinking alcohol if you’re on antibiotics. To ensure the best outcomes and minimize potential complications, it is recommended to follow the guidance provided by your healthcare professional or read the medication’s instructions and warnings regarding alcohol use during antibiotic treatment.
-
Can you mix antibiotics and alcohol?
Mixing antibiotics and alcohol is not advised. If you have plans to drink alcohol, it is advisable to wait until you have finished the prescribed antibiotics. Allow sufficient time for the antibiotics to be metabolized and eliminated from your system.
Alcohol Poisoning Symptoms, Signs, Cures, Effects & What To Do?
Can you drink alcohol while on antibiotics? While antibiotics themselves do not cause alcohol poisoning, some antibiotics can interact with alcohol in a way that may lead to unpleasant symptoms or exacerbate the effects of alcohol. The specific interactions between antibiotics and alcohol are determined by the type of antibiotic and the individual’s response.
However, it is generally advised to avoid alcohol consumption when taking antibiotics to reduce the risk of potential interactions. It’s best to consult with a healthcare professional or read the medication’s instructions and warnings for guidance regarding alcohol use while taking antibiotics.
Watch the video below to identify a case of alcohol poisoning. If you or a loved one is struggling with alcohol addiction or other substance use disorder(s), call for a FREE consultation 24/7 at (561) 678-0917
Get FREE addiction treatment insurance check – https://welevelup.com/rehab-insurance/
Alcohol Poisoning Symptoms Video Transcript.
Welcome to the We Level Up treatment center video series. In today’s video, we will discuss Alcohol Poisoning Symptoms, Signs, Cures, Effects & What To Do?
Drinking much alcohol quickly can have dangerous and fatal side effects, such as alcohol poisoning. A coma or death may result from too much alcohol too quickly, affecting respiration, heart rate, body temperature, and gag reflex.
Severe alcohol intoxication necessitates immediate medical attention. If you believe someone may have alcohol poisoning, call 911 to obtain immediate emergency medical care.
When to visit a doctor for alcohol poisoning?
Not all of the warning signs or symptoms of alcohol poisoning must occur before you seek medical help. It is important to note that patients with alcohol poisoning who are dozing off or who cannot be awakened risk dying.
Alcohol poisoning is an urgent situation.
If you have any suspicions, even if you don’t notice the classic symptoms or indicators of alcohol poisoning, you should get immediate medical help. What you need to do for alcohol poisoning is:
Dial your local emergency number or 911 right away. Never rely on someone recovering from alcohol poisoning to sleep.
Be prepared to share details. If you are aware, let medical staff or emergency workers know what kind, how much, and when the patient drank alcohol.
Never leave a person who is unconscious alone. Someone with alcohol poisoning may choke on their vomit and become unable to breathe because alcohol poisoning alters how the gag reflex functions. Don’t try to make the victim throw up while you wait for assistance; you risk making them choke.
Help someone who is throwing up. Make an effort to keep the person seated. Turn the person’s head to the side if they must lie down; this will help them from choking. To prevent unconsciousness, make an effort to keep the person awake.
Search We Level Up Antibiotics and Alcohol Detox, Mental Health Topics & Resources
Sources
[1] Mergenhagen KA, Wattengel BA, Skelly MK, Clark CM, Russo TA. Fact versus Fiction: Review the Evidence behind Alcohol and Antibiotic Interactions. Antimicrob Agents Chemother. 2020 Feb 21;64(3):e02167-19. DOI: 10.1128/AAC.02167-19. PMID: 31871085; PMCID: PMC7038249. Understanding Antibiotics and Alcohol Interaction.
[2] Ketoconazole. Product Information. Mylan Pharmaceuticals. Updated March 2018.
[3] Akdemir Kalkan İ, Çınar G, Pehlivanlı A, Ürkmez F, Topaloğlu İE, Akyol B, Onay Beşikçi A, Azap A, Memikoğlu KO. The pattern of systemic antibiotic use and potential drug interactions: Evaluations through a point prevalence study in Ankara University Hospitals. Turk J Med Sci. 2021 Apr 30;51(2):523-529. DOI: 10.3906/sag-2004-164. PMID: 32927931; PMCID: PMC8203144. Understanding Antibiotics and Alcohol Interaction.
[4] Understanding Antibiotics and Alcohol Interaction. (Antibiotics and Alcohol) Calhoun C, Wermuth HR, Hall GA. Antibiotics. [Updated 2022 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535443/
[5] Harmful Interactions & Alcohol’s Effects on Health – National Institute on Alcohol Abuse and Alcoholism (NIAAA) Understanding Antibiotics and Alcohol Interaction.
[6] Alcohol and Other Substance Use – Centers for Disease Control and Prevention (CDC) Understanding Antibiotics and Alcohol Interaction.
[7] Alcohol Use and Your Health – Centers for Disease Control and Prevention (CDC)
[8] Medicines To Treat Alcohol Use Disorder – Agency of Healthcare Research and Quality (AHRQ)
[9] Antibiotics: MedlinePlus – U.S. Department of Health and Human Services National Institutes of Health Understanding Antibiotics and Alcohol Interaction.
[10] Drug and Alcohol Use – Healthy People 2030 – Office of Disease Prevention and Health Promotion – Understanding Antibiotics and Alcohol Interaction.